Introduction
Emotion regulation refers to strategies used to identify, initiate and modify the course of emotions (1–3). Emotion regulation strategies can be automated or controlled methods used to cope with or modify the external expression and/or internal experience when the emotional state has unwanted impact on a desired outcome (1–3). For example, a young person might suppress their feelings of sadness when moving away from their childhood home in an attempt to not upset their parents thus reducing the external expression of negative emotions. They might then remind themselves they can still visit their parents in an attempt to gain more perspective, reappraise, and reduce the internal experience of sadness. A theoretical framework based on the emotion regulation process model has proposed that emotion regulation strategies can be broadly divided into adaptive and maladaptive strategies (4–7). The adaptive strategies include reappraisal, active problem solving, and mindfulness strategies based on awareness and acceptance of emotions, while the maladaptive strategies include rumination, avoidance, and suppression of emotions (4–6). Although the maladaptive strategies can be useful in some scenarios, this framework focuses on dispositional emotion regulation. Thus, for a given strategy to be considered adaptive is needs to be effective and helpful across contexts (6). Excessive reliance on maladaptive strategies has been found to be linked to anxiety symptoms and to impact treatment response in anxiety disorders (4, 5). Similarly, people with eating disorders (EDs) have been reported to rely more on maladaptive than adaptive emotion regulation strategies (8–10). Thus, this review will focus on further investigating the associations between different adaptive and maladaptive emotion regulation strategies an ED psychopathology.
Over the years there has been a great deal of interest in exploring emotion regulation within EDs; it has been proposed that difficulties in emotion regulation is one of the social-emotional factors contributing to the development and maintenance of disordered eating (9, 11–13). Large scale systematic reviews and meta-analyses have reported links between ED symptomatology and dispositional tendency toward maladaptive emotion regulation and emotion dysregulation among people with anorexia nervosa (AN), bulimia nervosa (BN), and binge eating disorder (BED), both when assessed under laboratory conditions and under naturalistic conditions in studies using ecological momentary assessments (EMAs) (9, 11, 13). Recently a meta-analytic review by Prefit et al. (12) examined correlations between the use of various emotion regulation strategies and ED psychopathology across all ED diagnoses. The authors focused on examining individual adaptive strategies, including emotional awareness, clarity about emotions, acceptance of emotions, cognitive reappraisal, and problem solving, as well as maladaptive strategies, such as avoidance, rumination and suppression of emotions. The findings showed that across the board maladaptive emotion regulation strategies were positively associated with ED symptoms while the use of adaptive strategies was negatively associated with ED psychopathology. Interestingly, this was the case across ED diagnoses and the authors found no significant evidence of group differences in the analyses. Additionally, no particular strategy came out as more closely associated with ED psychopathology, instead it appeared that all adaptive strategies were equally negatively associated and all maladaptive strategies were equally positively associated with ED symptomatology.
Although the findings from previous reviews highlight the interesting associations between emotion regulation difficulties and ED psychopathology, whether there is a particular aspect of adaptive or maladaptive emotion regulation that has a most important role in EDs remains unclear. This question could be approached using the network meta-analysis technique, which explores comparative associations of several emotion regulation strategies by utilizing existing direct evidence to estimate indirect evidence. This approach has been previously used to compare different interventions to identify most effective treatments (14–17). More recently the network meta-analysis approach has also been used to compare associations in the field of educations (18). The authors demonstrated a method of applying network meta-analysis to investigate which test was the most closely associated with pupils reading fluency, in an attempt to identify the most useful reading test to be used in school setting. Such a methods could also be applied to emotion regulation in EDs to identify if there is a particular strategy that is most closely associated with ED symptomatology. This approach could inform the development of novel interventions for EDs rather than aiming to generally increase the use of adaptive strategies and reduce reliance on maladaptive strategies.
The aim of this meta-analytic review was to build on and synthesize previous literature by comparing findings from previous work examining the association between different aspects of adaptive and maladaptive emotion regulation and ED psychopathology among people with a diagnosis of an ED. Thus, this review aimed to build on the recent work by Prefit et al. (12) and conduct a network meta-analysis. We compared the use of adaptive emotion regulation strategies, including acceptance of emotions, awareness of emotions, problem solving, and cognitive reappraisal, as well as maladaptive emotion regulation strategies, such as avoidance, rumination, and emotion suppression. The objective was to identify aspects of emotion regulation that have closest association with ED symptomatology to identify useful targets for therapeutic interventions. As previous work has suggested that difficulties in emotion regulation may be trans-diagnostic (12, 13), we assessed the associations between the use of different emotion regulation strategies and ED symptomatology across ED diagnoses. Because findings from previous meta-analyses have reported very similar associations between different emotion regulation strategies and ED symptomatology, we did not have a priori expectations regarding which one or more emotion regulation strategies would emerge as being most closely associated with ED psychopathology.
Materials and Methods
Literature Search
The following keywords were used to search electronic databases including PsychINFO, PsychARTICLES, Medline, Scopus, Pubmed, and Web of Knowledge: (“eating disorder” OR “anorexia nervosa” OR “bulimia nervosa” OR “binge eating disorder”) AND (“emotion regulation” OR “emotion dysregulation” OR “affect regulation” OR “affect dysregulation” OR “avoidance” OR “suppression” OR “rumination” OR “problem solving” OR “problem coping” OR “awareness” OR “mindfulness” OR “acceptance” OR “clarity” OR “appraisal” OR “reappraisal”). Where possible filters were used to exclude animal studies, case reports, reviews, and studies not published in English. The initial search was conducted in April 2021 and was updated in August 2021. Bibliographies of included papers and the previous review by Prefit et al. (12) were searched to identify any studies missed in the initial search.
Inclusion Criteria
To be included in the review the studies were requires to meet the following inclusion criteria: (1) include a group of adults or adolescents [10–19 years old (19)] with a diagnosis of an ED, (2) measure some aspect of emotion regulation, (3) measure ED symptomatology, (4) be published in English, and (5) be published in a peer reviewed journal. In the case of longitudinal or interventional studies, only emotion regulation and ED symptomatology measures taken at baseline or pre-treatment were included. Additionally, studies that only assessed emotion regulation and/or ED symptomatology at a later stage, post-intervention or at treatment follow-up, were excluded. As we were interested in comparing different emotion regulation strategies, any studies that reported only overall measures and did not assess a specific aspects of emotion regulation were not included. Studies that instructed participants to use specific emotion regulation strategies or assessed regulation of eating or other aspects of food intake, or emotion regulation related behaviors that were to do with food, eating or bodies, such as food avoidance, or body image acceptance, were also excluded. Finally, studies that included young children or clinical populations with diagnoses other than an ED were excluded.
Study Selection
This review was conducted in accordance with the PRISMA guidelines and the flow diagram detailing the literature search and study selection is presented in Figure 1. The initial search and screening based on title and abstract was conducted by J.L along with H.M. The included full text articles were then assessed for eligibility and decisions about final inclusion or exclusion of articles was made initially by the first author. All excluded papers were screened again based on title and abstract by H.M. to ensure no relevant studies were missed. In case uncertainty regarding whether a given study should be included or excluded, the full text article was brought to the rest of the team for consensus meeting and team discussion.
Figure 1. Flow diagram. ED, Eating disorder; EMA, ecological momentary assessment.
Data Collection and Synthesis
To conduct the network meta-analysis, we took a similar approach to a recent review investigating associations between oral reading fluency and text complexity measures to identify an assessment method most closely correlated with reading fluency (18). Thus, correlation coefficient between an emotion regulation measure and ED symptomatology was extracted from all included papers along with the ED group sample size, the aspect of emotion regulation assessed, and the type of ED symptomatology measure used. Only correlation analysis conducted within the ED group were included. If only correlations for the whole sample which included healthy participants or participants with other diagnoses were reported, the corresponding author was contacted to obtain access to a within ED group correlation coefficient. If a study included more than one ED group separate correlation coefficients for each diagnostic group or one correlation coefficient for the whole mixed ED group were included depending on what was reported. We did not favor separate correlation coefficients as the meta-analysis included all ED diagnoses. The relevant correlation coefficients were not reported in the main text or Supplementary Materials of 267 studies and the corresponding authors were contacted by D.B. to gain access to the data. Correlation coefficients which were not reported in 28 of the included manuscripts, were obtained through personal correspondence. Additional data regarding the age of the ED group, body mass index (BMI), and percentage of female participants was also extracted where available.
Methods Used to Assess Emotion Regulation
We included studies that assessed the use of adaptive emotion regulation strategies, including reappraisal, acceptance of emotions, emotional awareness, and problem solving, as well as the use of maladaptive emotion regulation strategies, such as avoidance, suppression, and rumination (4–7).
Adaptive Emotion Regulation Measures
Thirty-one studies assessed the association between acceptance of emotions and ED symptomatology. Four different methods were used to assess acceptance of emotions (see Table 1 for details), all of which were self-report questionnaire measures. The most commonly used measure was the Difficulties in Emotion Regulation Scale [DERS; (123)] non-acceptance subscale (N = 24). For the purposes of the meta-analysis all correlation coefficients had to have the same direction, with positive correlations indicating that a greater level of ED symptomatology was associated with more difficulties in emotion regulation. Therefore, the correlations that included measures of acceptance of emotions were reversed, while correlation that included measures of non-acceptance or difficulties in accepting emotions were not reversed. This was done to reflect reverse scoring of adaptive emotion regulation, whereby higher scores indicate less acceptance and, thus, this review assessed associations between non-acceptance of emotions and ED symptomatology.
Table 1. Study characteristics.
Thirty-eight studies examined associations between emotional awareness and ED symptomatology. Nine different measures were used to assess awareness of emotions (Table 1), eight of which were self-report questionnaire measures. The most commonly used measure was the DERS lack of emotional awareness subscale (N = 24). One of the measures used, the Levels of Emotional Awareness, is a performance based measure assessing participants’ awareness of their own and other’s emotions. Although this review builds on the previous meta-analytic review by Prefit et al. (12) we did not include emotional clarity as a separate category. We found that very few measures assessed clarity and those that did used methods that were very similar to ones used to evaluate emotional awareness. For instance the Attention and Clarity of One’s Feelings and the Feelings of Others (ACF) questionnaire is described as measuring emotional self-awareness and includes questions about a persons awareness of and clarity about their own emotions. Therefore, for the sake of simplicity, emotional awareness and clarity were combined and in the case of the DERS questionnaire, which assesses both separately, only the lack of emotional awareness subscale was used. Studies assessing mindfulness were also combined with those investigating emotional awareness and clarity as the measures used were deemed to be very similar, examining similar underlying construct of paying attention to one’s feelings and knowing what are the emotions one is feeling. As above, the correlations that included measures of emotional awareness, were reversed, while those that included measures of lack of awareness or difficulties in emotional awareness were kept as is. Therefore, this review ended up assessing associations between lack of emotional awareness and ED symptomatology.
Thirty-four studies examined associations between the impact of emotions on participant’s problem solving abilities and ED symptomatology (Table 1). Six different measures were used to assess problem solving, four of which were self-report questionnaires and the most commonly used measure of problem solving was the DERS difficulties with goal directed behaviors subscale (N = 24). One of the measures, the Means-Ends Problem-Solving Test [MEPS; (124)], was a performance-based measure used to evaluate the effectiveness of participants problem solving strategies. In this task participants are given the beginning and end of four different scenarios and they are then asked to provide the middle part connecting the beginning and ending. In all but two of the measures a higher score indicated better problem solving and thus, the correlation coefficients were reversed for the meta-analysis to assess association between problem solving difficulties and ED symptomatology. The Social Problem-Solving Inventory-Revised [SPSI-R; (125)] includes the negative problem orientation subscale and the DERS includes difficulties with goal directed behaviors subscale, both of which assess negative approach that prevents effective problem solving. This subscale was used in the present review.
Eight studies examined associations between cognitive reappraisal of emotions and ED symptomatology (Table 1). Two different measures were used to assess cognitive reappraisal, both of which were self-report questionnaires and the most commonly used measure was the Emotion Regulation Questionnaire [ERQ; (126)] reappraisal subscale (N = 5). In both questionnaires, higher scores indicated greater use of cognitive reappraisal and thus, the correlation coefficients were reversed to assess associations between lack of cognitive reappraisal and ED symptomatology.
Maladaptive Emotion Regulation Measures
Forty-seven studies investigated associations between emotional avoidance and ED symptomatology (Table 1). Twenty-one different measures were used to assess emotional avoidance, 16 of which were self-report questionnaires; the most commonly used measure was the Temperament and Character Inventory [TCI; (127)] harm avoidance subscale (N = 13). One of the measures, the Anagram solution task, used a behavioral measure of avoidance of threatening words. In this task, participants were given a set of anagrams to solve and the time taken to reach the correct solution was used to measure avoidance. In all measures, higher scores indicated more avoidance.
Seven studies examined associations between rumination and ED symptomatology (Table 1). Four different measures were used to assess rumination, all of which were self-report questionnaires. The most commonly used measure to assess rumination was the Ruminative Response Scale [RSS; (128)] (N = 5). One of the questionnaires used was adapted from the RSS to assess ED specific rumination (46). In all measures used, higher scores indicated more rumination.
Thirteen studies investigated association between emotion suppression and ED symptomatology (Table 1). Six different measures were used to assess emotion suppression, five of which were self-report questionnaires and the most commonly used measure was the only task-based assessment, which examined evoked facial affect (N = 5). In the Evoked facial affect task, participants were presented with emotionally provoking stimuli and their evoked facial expressions were analyzed. In this task, higher scores indicated more emotion expression and less suppression, and thus, the correlation coefficients were reversed to reflect reverse scoring of the task. In all self-report measures, higher scores indicated more emotion suppression.
Quality Assessment
Quality assessment was conducted by J.L. and D.B. using the NIH Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools) to investigate study level bias and the results are shown in Supplementary Data. Question relating to exposures were not considered as they were not relevant for the purpose of the present review, which focused on correlations prior to any potential interventions or exposures. Inter-rater reliability was good [intra-class correlation coefficient = 0.94, 95% CI (0.93, 0.96)]. Any disagreements were resolved through group discussion. All included studies were deemed to be high enough quality to be included in the meta-analysis and the sum of the quality scores were included in a meta-regression to examine whether the study quality could explain any potential network inconsistency.
Statistical Analysis
We conducted a Bayesian network meta-analysis to examine which aspects of emotion regulation were most closely associated with ED symptomatology. The meta-analysis was conducted in R (129) using the packages gemtc (130) and metafor (131). First, all relevant correlation coefficients of the association between an aspect of emotion regulation and ED symptomatology were extracted from the included studies. The Pearson’s r coefficients were then adjusted using sample-size weights to approximate population correlation and Fisher’s r-to-z transformed was conducted using the function escalc from the package metafor. We converted the correlation coefficients to z-scores for the purposes of the network meta-analysis as z-scores are not bounded and come from a normal distribution. We then calculated standard error for each study from the sample size adjusted variance using the following steps
where v is the estimated, sample size adjusted variance, σ is the standard deviation, and n is the sample size. The sample size adjusted correlation coefficients and standard errors were then taken forward to conduct the network meta-analysis.
First, we generated an initial network of the data where edge thickness represents the number of studies that reported that correlation. The generated network object was then taken forward to specify and compile the random effects model with four Markov chains and a normal likelihood function with an identity link. Next, a Markov Chain Monte Carlo (MCMC) simulation was conducted to estimate the posterior probabilities. To ensure convergence we specified 1,00,000 iterations with 5,000 burn-in iterations. The Gelman-Rubin plots are presented in Supplementary Figure 1. The parameter estimation is conducted by utilizing Just Another Gibbs Sampler (JAGS). We then generated rank probability and forest plots to visualize the direct comparisons between different aspects of emotion regulation and to examine which aspect was the most closely associated with ED symptomatology. Additionally, we also calculated Surface Under the Cumulative Ranking (SUCRA) score to evaluate which aspect of emotion regulation is most relevant in terms of ED symptomatology and might serve a useful target for interventions.
Network inconsistency was examined using a network splitting method and node comparisons with Bayesian p
This review has been registered on PROSPERO (ID: CRD42021249996) and the code and data used to conduct the meta-analysis is available on the Open Science Framework online repository (https://osf.io/gz3kt/?view_only=6fe361c208e04817b820c1f3fb2fd2b5).
Results
Study Characteristics
The characteristics of each study included in the review are summarized in Table 1. Altogether, data from 19,734 participants were included in the meta-analysis, with average study sample size of 181 (range = 6–2,405). Majority, 72, of the studies included only female participants and three studies did not report the participants’ gender. Additionally, most studies included a mixed ED sample and assessed emotion regulation across ED diagnoses while 50 studies examined emotion regulation within one diagnostic group. The mean age across studies was 27.7 (range = 15.0–49.3); most studies included adults and only eight studies included a sample of adolescents with sample mean age below 18. The mean BMI across studies was 22.25 (range = 14.6–39.7), with most studies including people who were of healthy weight, and 29 studies including underweight participants with sample mean BMI below 18.5 and 15 studies including overweight participants with sample mean BMI above 25.
Network Characteristics
The initial network graph, in Figure 2, shows the eligible comparisons to identify emotion regulation strategy most strongly linked to ED symptomatology. The thickness of the edges indicates the number of studies that evaluated a given association or comparison. In the present review most of the studies (N = 50) examined the association between avoidance and ED symptomatology. Across the 104 included studies, 294 correlations contributed to the network. All emotion regulation strategies were compared with at least one other emotion regulation method in addition to the association with ED symptoms resulting in a well-connected network, which is more likely to produce reliable results (132).
Figure 2. Initial network plot. Line thickness represents the number of studies reporting the association.
Forest Plot
The forest and SUCRA plots from the Bayesian random effects network meta-analysis are shown in Figure 3. Each emotion regulation strategy represents a unit of analysis and is thus presented on the rows. Larger positive effect sizes indicate a stronger association between a given emotion regulations strategy and ED symptomatology. The meta-analysis showed that the emotion regulation strategies vary in their relationship with ED symptomatology, with two methods showing the strongest association: rumination [ES = 0.51, 95% CrI (0.33, 0.69)] and non-acceptance of emotions [ES = 0.43, 95% CrI (0.35, 0.51)]. Lack of cognitive reappraisal had the weakest association with ED psychopathology [ES = 0.17, 95% CrI (0.02, 0.34)].
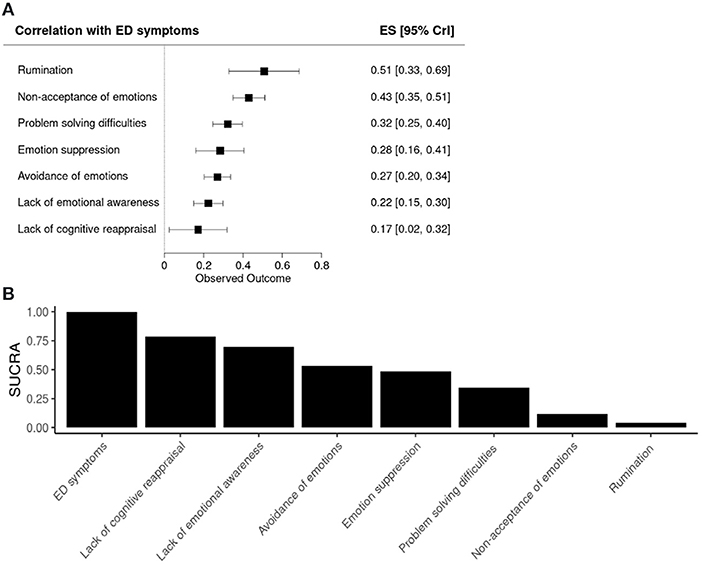
Figure 3. Forest and SUCRA plots. (A) Forest plot showing the associations between the emotion regulation strategies and ED symptoms. (B) Bar plot showing the surface under the cumulative ranking (SUCRA) for each emotion regulation method. ES, effect size; CrI, Credible Interval.
Meta-Regressions
Network inconsistency was evaluated using the node-split method (Supplementary Figure 2). Although there was no evidence of significant inconsistency, the comparisons between problem solving difficulties and lack of emotional awareness (p = 0.076) and rumination and non-acceptance of emotions (p = 0.084) approached significance. Therefore, three meta-regressions were conducted to examine whether these slight inconsistencies could be explained between-study differences in study quality score, BMI, age, or whether the study included only female participants or a mixed sample of participants. The meta-regressions revealed a significant effect of BMI [b = −0.09 CrI (−0.18, −0.01)] such that the associations between different emotion regulation strategies and ED psychopathology were weaker among those with low BMI. There was no significant effect of study quality [b = −0.01, CrI (−0.09, 0.12)], age (b = −0.04, CrI (−0.14, 0.06)] or whether the studies included of only female or mixed participants [b = 0.02, CrI (−0.12, 0.32)].
Discussion
The aim of the present review was to examine associations between various adaptive and maladaptive emotion regulation strategies and ED psychopathology trans-diagnostically to identify strategies that were most closely linked with psychopathology. We used network meta-analysis approach with a well-connected network, which identified rumination and non-acceptance of emotions to be most closely associated with ED symptomatology. Difficulties in cognitive reappraisal was found to be the least connected with ED symptomatology of all emotion regulation strategies examined in this review. There was some evidence of network inconsistency which approached significance and two meta-regressions were performed to examine if this could be explained by the between-study variability in BMI or age. The meta-regressions were non-significant suggesting the findings were consistent across age groups and BMI.
The present review adds to the steady accumulation of evidence highlighting the relationship between maladaptive emotion regulation based on rumination and ED symptomatology (133, 134). Over the recent years, studies using ecological momentary assessments (EMAs) have reported that rumination and repetitive negative thinking predicts engagement in ED behavior, including body checking and binge eating (135–137). One EMA study also reported that excessive rumination also predicted higher levels of ED psychopathology at a 1 month follow-up assessment (135). Moreover, it has been suggested that some ED symptoms, such as excessive focus on food, eating, and body weight and shape, are forms of illness specific rumination (138). Indeed, a longitudinal study using EMA and biological assessments found that food-related rumination was linked to BMI status and leptin levels among people in treatment for anorexia nervosa (139). This suggest that at least certain aspects of illness-specific rumination may be linked to under-nutrition and physiological signaling, explaining why weight restoration can have a positive impact on this type of rumination. Overall, it appears that rumination, whether general repetitive negative thinking or illness-specific, is a key characteristic of the acute stage of an ED.
It is important to note that most of the studies included in the present review used the RRS questionnaire, which assesses brooding, depressive rumination, and reflection. Therefore, it is possible that the observed strong association between rumination and ED psychopathology may be partially explained by known links between depression and ED symptoms (140, 141). Indeed, one study reported that although food-related rumination was linked to stage of illness and under-nutrition, other aspects of illness-specific rumination including, body weight and shape, were more associated with negative mood than not ED symptoms (139). Additionally, an experimental study has reported that induction of body shape related rumination had a direct negative impact on mood but not on ED cognitions among people with BED (142). Another interpretation is that the above findings may reflect the mechanism through which rumination influences EDs: due to its repetitive nature of rumination forms a habitual relationship with depressive mood which in turn fuels ED symptomatology (143). In support of this hypothesis, one longitudinal EMA study documented a bidirectional mediation between rumination, negative mood, and ED symptoms (136). The authors found that rumination mediated the association between low mood and ED symptomatology and low mood in turn mediated the association between rumination and ED symptomatology. Taken together these findings highlight the need to further examine the underlying processes through which rumination impacts EDs and how rumination may impact illness progression and recovery.
Difficulties in adaptive emotion regulation, specifically with accepting emotions, was another domain that was highly associated with ED psychopathology in the present review. This is in line with findings from the general population showing that reduced use of adaptive emotion regulation strategies, such as acceptance, and increased reliance on maladaptive methods, including suppression and avoidance, are associated with daily habit of food restriction (144). Similarly, people who report objective binge eating episodes and loss of control over eating also report more difficulties accepting emotions than those who do not engage in disorder eating behaviors (145). Additionally, a recent longitudinal study reported that a poor response to CBT-based ED treatment was associated with lack of change in the patients’ self-reported ability to accept emotions and limited access to other effective emotion regulation strategies (146). Moreover, another interventional study found that irrespective of treatment condition, changes in acceptance of emotions were associated with greater improvements in ED-related quality of life post-intervention (27). These findings have led some authors to suggest that emotion regulation in general and acceptance of unwanted emotions in particular should be added to current standard ED treatments (146, 147). While it seems that acceptance of emotions may have a strong role in disordered eating and the progression of EDs, further investigation of the underlying mechanism would be of interest to aid the development of evidence-based interventions.
Interestingly, difficulties accepting emotions has also been proposed to be linked to excessive reliance on other maladaptive emotion regulation strategies, including rumination, avoidance, and suppression (148, 149). If unwanted emotions are deemed unacceptable, a person might put great effort in avoiding situations that give rise to such emotions or, if the emotions are already present, engage in suppression in an attempt to manage the unwanted emotions. Findings from a review of experimental and self-report studies support this notion reporting links between suppression and non-acceptance of emotion among people with AN and BN (150). Difficulties accepting and general dislike of emotions have been linked to greater general tendency to engage in rumination as well as worry and low mood (151). Interestingly, difficulties in emotion regulation, including non-acceptance of emotions, have been found to mediate the association between experiential avoidance and ED psychopathology among people with a range of ED diagnoses (44). Similar findings have been reported in the general population with reduced access to adaptive emotion regulation strategies, including acceptance of emotions and reappraisal, and increased reliance on maladaptive strategies based on suppression being associated with greater tendency to engage in ED-related behaviors (144). Thus, further investigation of the mechanisms that might underlie this connection as well as examination of the impact of acceptance-focused interventions on the use of other emotion regulation strategies among people with EDs may be of interest.
Interestingly, our meta-regression also found a significant effect of BMI, such that the associations were generally weaker among those with lower BMI. This is somewhat in contrast with previous reviews suggesting that there are no significant differences in the associations between emotion regulation methods and ED psychopathology between different ED diagnostic groups characterized by low and high BMI (12, 13). However, some studies have reported that starvation impacts emotion regulation in such a way that those with very low BMI in the acute stage of AN report fewer difficulties (152). Indeed, it has been suggested that self-starvation itself works as an emotion regulation strategy which reduces both the internal experience and external expression of emotions through (153). By suppressing physiological responses and arousal, starvation can help the person escape and avoid unwanted emotions (153, 154). If no alternative methods are available, the person may over time become reliant on starvation as their sole emotion regulation strategy due to its numbing effect (155, 156). This mechanism could be one of the factors contributing to the present finding and it further highlights the complex relationship between emotion regulation and EDs.
Clinical Implications
Over the recent years, several reviews have recommended the use of interventions aimed at reducing rumination and repetitive negative thinking, Metacognitive Therapy (MCT) and Rumination-Focused Cognitive Behavioral Therapy (RFCBT), such as in the treatment of EDs (10, 12, 133, 134). MCT and RFCBT have been successfully used to treat anxiety and depression among other psychiatric disorders, and there is some evidence suggesting that rumination-focused treatments may help reduce the risk of relapse in depression (157–159). Furthermore, one of the meta-analytic reviews found a very high correlation between rumination and ED symptomatology among the general population, which led the authors to suggest that rumination may be a useful target for interventions aiming to prevent EDs and other forms of disordered eating (133). To date, very few studies examining the impact of interventional designed to target rumination in EDs have been conducted. To our knowledge only one case series has explored the effects of MCT on binge eating behavior among three people with BED (160). MCT aims to alleviate repetitive negative cognitions by increasing awareness and mindfulness, and modifying the metacognitions that underlie maladaptive behaviors, such as binge eating (161, 162). The Robertson and Strodl (160) found that MCT intervention significantly reduced binge eating frequency and improved cognitions related worry and rumination. There improvements were maintained at a 2-month follow-up assessment. Together, these findings highlight the need to develop new interventions or adapt existing treatments to target rumination and repetitive negative thinking in EDs.
Acceptance and mindfulness based interventions, such as Acceptance and Commitment Therapy (ACT), have been proposed to target difficulties in coping with unwanted emotions in EDs (147, 163). The purpose of ACT is to encourage people to accept and experience unwanted emotions without attempts to modify them, thus reducing avoidance and suppression of difficult emotions and embracing the use of adaptive emotion regulation strategies (163). A number of small case series have reported that ACT can be effective in reducing ED symptomatology and behaviors among people with AN and BED (164–166). Another larger longitudinal treatment study found that ACT was more effective than treatment as usual in reducing residual ED symptoms and risk or relapse following standard ED treatment and the effects were maintained at a 2-year follow-up (167). However, another interventional study found that ACT did not lead to greater improvements in ED related quality of life than treatment as usual (27). Furthermore, a systematic review examining the use of ACT to treat body image disturbance and weight dissatisfaction reported that they could not determine the effectiveness of ACT due to the poor quality of current evidence (168). These findings suggest that acceptance and mindfulness based interventions may be promising in the treatment of EDs, but more research into the mechanisms that underlie the relationship between emotion acceptance and ED psychopathology is needed to create evidence-based treatment strategies.
Limitations
The main limitation of this review was the use of the network meta-analysis due to its use of indirect evidence, which relies on the assumption of transitivity (169). According to the transitivity assumption, a given associations is exchangeable between studies even if a given study did not assess that association. This assumption can be violated by individual differences in the samples between studies, which can be difficult to control resulting in network inconsistency. Although we did not observe significant network inconsistency, there was evidence of near significant inconsistency in two comparisons. Moreover, since we used the network approach to meta-analysis we were able to only include studies that reported correlation coefficients, which led to the exclusion of a substantial number of otherwise relevant studies. Although we attempted to contact the corresponding authors of all papers which did not report the relevant data, we were able to gain access to correlation coefficients from only 28 studies through personal correspondence. Including only a subset of the available literature to the meta-analysis may have impacted the findings.
Another limitation of this review is that majority of the studies included adult women with normal BMI. Although the meta-regressions indicated that age did not have a significant impact on the results, findings from the present review may not be fully generalizable to all age groups. Additionally, even though we did find a significant effect of BMI, we were not able to examine the impact of diagnostic group as the gemtc package used in the present analysis does not presently handle categorical covariates. To truly examine the potential transdiagnostic nature of emotion regulation difficulties in EDs, a direct comparison of different diagnostic groups would be needed rather than solely focusing on BMI. Furthermore, the findings may not be fully generalisable to other genders. Gender identity can impact a person’s experiences with the world around them and thus influence their emotion regulation habits (170, 171). Thus, further exploration of the impact of gender and particularly minority gender identity on emotion regulation in EDs is needed. Finally, it is also important to note that we did not have equal number of studies examining each association. Indeed, only eight studies reported correlations involving difficulties with cognitive reappraisal and this method was found to be most weakly associated with ED psychopathology with largest between study variance. It is possible that this finding may have been impacted by the small number of studies included. However, only seven studies reposted correlations involving rumination and this maladaptive strategy was found to be most strongly associated with ED psychopathology. Still, equal and large number of studies examining each association would enable us to draw stronger conclusions.
Conclusions
This review aimed to build on previous work by conducting a trans-diagnostic network meta-analysis to identify emotion regulation strategies most closely associated with psychopathology among those with ED. The meta-analysis revealed that rumination and difficulties accepting emotions were most closely associated with ED symptoms, while the weakest association was between difficulties with cognitive reappraisal and ED symptoms. The meta-regressions showed that BMI had significant impact such that the associations between various emotion regulation strategies and ED psychopathology were weaker among those with low BMI. The present findings add to the steady accumulation of evidence highlighting the relationship between ED psychopathology and reliance on maladaptive emotion regulation strategies based on rumination and non-acceptance of emotions. Together with previous longitudinal observational studies and ecological momentary assessments, these findings suggest that these two maladaptive strategies may have a key role in maintaining and perpetuating ED. The meta-regression finding also emphasizes the complex relationship between ED symptoms and emotion regulation. It is possible that some people with ED may use starvation and malnutrition to escape and avoid unwanted emotions. Thus, there is pressing need to explore and develop interventions targeting emotion regulation difficulties in ED with particular focus on rumination and non-acceptance of emotions.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: https://osf.io/gz3kt/?view_only=6fe361c208e04817b820c1f3fb2fd2b5.
Author Contributions
JL: conceptualization, methodology, investigation, formal analysis, visualization, writing—original draft, and writing—review and editing. DB and HM: methodology, investigation, validation, and writing—review and editing. SW and KT: conceptualization, writing—review and editing, and supervision. All authors contributed to the article and approved the submitted version.
Funding
This research was funded in whole, or in part, by the Wellcome Trust [213578/Z/18/Z]. For the purpose of open access, the author has applied a CC BY public copyright licence to any Author Accepted Manuscript version arising from this submission. The research was further supported by MRC-MRF Fund [MR/R004595/1]. The funding bodies did not play an active role in the design of this study, nor in data collection or analysis, nor in writing the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.793094/full#supplementary-material
References
1. Gross JJ. The emerging field of emotion regulation: an integrative review. Re Gen Psychol. (1998) 2:271–99. doi: 10.1037/1089-2680.2.3.271
CrossRef Full Text | Google Scholar
2. Gross JJ. Emotion Regulation: Affective, Cognitive, and Social Consequences. Psychophysiology. Cambridge: Cambridge University Press (2002).
PubMed Abstract | Google Scholar
3. Gross JJ, Thompson RA. “Emotion regulation: conceptual foundations,” in Handbook of Emotion Regulation. New York, NY: The Guilford Press (2006).
PubMed Abstract | Google Scholar
4. Aldao A, Jazaieri H, Goldin PR, Gross JJ. Adaptive and maladaptive emotion regulation strategies: interactive effects during CBT for social anxiety disorder. J Anxiety Disord. (2014) 28:382–9. doi: 10.1016/j.janxdis.2014.03.005
PubMed Abstract | CrossRef Full Text | Google Scholar
6. Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev. (2010) 30:217–37. doi: 10.1016/j.cpr.2009.11.004
PubMed Abstract | CrossRef Full Text | Google Scholar
8. Mason TB, Smith KE, Anderson LM, Tyler H, Smith KE, Anderson LM, et al. Anhedonia, positive affect dysregulation, and risk and maintenance of binge-eating disorder. Int J Eat Disord. (2021) 54:287–92. doi: 10.1002/eat.23433
PubMed Abstract | CrossRef Full Text | Google Scholar
9. Oldershaw A, Lavender T, Sallis H, Stahl D, Schmidt U. Emotion generation and regulation in anorexia nervosa: a systematic review and meta-analysis of self-report data. Clin Psychol Rev. (2015) 39:83–95. doi: 10.1016/j.cpr.2015.04.005
PubMed Abstract | CrossRef Full Text | Google Scholar
10. Trompeter N, Bussey K, Forbes MK, Mitchison D. Emotion dysregulation within the CBT-E model of eating disorders: a narrative review. Cogn Ther Res. (2021) 45:1021–36. doi: 10.1007/s10608-021-10225-5
CrossRef Full Text | Google Scholar
13. Puttevils L, Vanderhasselt M-A, Horczak P, Vervaet M. Differences in the use of emotion regulation strategies between anorexia and bulimia nervosa: a systematic review and meta-analysis. Compr Psychiatry. (2021) 109:152262. doi: 10.1016/j.comppsych.2021.152262
PubMed Abstract | CrossRef Full Text | Google Scholar
14. Cuijpers P, Noma H, Karyotaki E, Vinkers CH, Cipriani A, Furukawa TA. A network meta-analysis of the effects of psychotherapies, pharmacotherapies and their combination in the treatment of adult depression. World Psychiatry. (2020) 19:92–107. doi: 10.1002/wps.20701
PubMed Abstract | CrossRef Full Text | Google Scholar
15. Davies C, Cipriani A, Ioannidis J, Radua J, Stahl D, Provenzani U, et al. Lack of evidence to favor specific preventive interventions in psychosis: a network meta-analysis. World Psychiatry. (2018) 17:196–209.doi: 10.1002/wps.20526
PubMed Abstract | CrossRef Full Text | Google Scholar
16. Landoni G, Greco T, Biondi-Zoccai G, Nigro Neto C, Febres D, Pintaudi M, et al. Anaesthetic drugs and survival: a Bayesian network meta-analysis of randomized trials in cardiac surgery. Br J Anaesth. (2013) 111:886–96. doi: 10.1093/bja/aet231
PubMed Abstract | CrossRef Full Text | Google Scholar
17. Padwal R, Klarenbach S, Wiebe N, Birch D, Karmali S, Manns B, et al. Bariatric surgery: a systematic review and network meta-analysis of randomized trials. Obes Rev. (2011) 12:602–21. doi: 10.1111/j.1467-789X.2011.00866.x
PubMed Abstract | CrossRef Full Text | Google Scholar
18. Saha N, Cutting L. Exploring the use of network meta-analysis in education: examining the correlation between ORF and text complexity measures. Ann Dyslexia. (2019) 69:335–54. doi: 10.1007/s11881-019-00180-y
PubMed Abstract | CrossRef Full Text | Google Scholar
19. Vanderkruik R, Gonsalves L, Kapustianyk G, Allen T, Say L. Mental health of adolescents associated with sexual and reproductive outcomes: a systematic review. Bull World Health Organ. (2021) 99:359–73K. doi: 10.2471/BLT.20.254144
PubMed Abstract | CrossRef Full Text | Google Scholar
20. Brytek-Matera A, Schiltz L. Comparative structural study of the configuration of coping strategies among female patients with eating disorders and a non-clinical control group. Psychiatr Danub. (2013) 25:365.
PubMed Abstract | Google Scholar
21. Aloi M, Rania M, Carbone EA, Calabrò G, Caroleo M, Carcione A, et al. The role of self-monitoring metacognition sub-function and negative urgency related to binge severity. Eur Eat Disord Rev. (2020) 28:580–6. doi: 10.1002/erv.2742
PubMed Abstract | CrossRef Full Text | Google Scholar
22. Aloi M, Rania M, Carbone EA, Caroleo M, Calabrò G, Zaffino P, et al. Metacognition and emotion regulation as treatment targets in binge eating disorder: a network analysis study. J Eat Disord. (2021) 9:22. doi: 10.1186/s40337-021-00376-x
PubMed Abstract | CrossRef Full Text | Google Scholar
23. Blomquist KK, Roberto CA, Barnes RD, White MA, Masheb RM, Grilo CM. Development and validation of the eating loss of control scale. Psychol Assess. (2014) 26:77. doi: 10.1037/a0034729
PubMed Abstract | CrossRef Full Text | Google Scholar
24. Bodell LP, Pearson CM, Smith KE, Cao L, Crosby RD, Peterson CB, et al. Longitudinal associations between emotion regulation skills, negative affect, and eating disorder symptoms in a clinical sample of individuals with binge eating. Eat Behav. (2019) 32:69–73. doi: 10.1016/j.eatbeh.2018.12.005
PubMed Abstract | CrossRef Full Text | Google Scholar
25. Brown TA, Berner LA, Jones MD, Reilly EE, Cusack A, Anderson LK, et al. Psychometric evaluation and norms for the Multidimensional Assessment of Interoceptive Awareness (MAIA) in a clinical eating disorders sample. Eur Eat Disord Rev. (2017) 25:411–6. doi: 10.1002/erv.2532
PubMed Abstract | CrossRef Full Text | Google Scholar
26. Hazzard VM, Peterson CB, Crosby RD, Schaefer LM, Smith KE, Engel SG, et al. Predictors of treatment response durability in psychotherapy for binge-eating disorder: Examining the roles of self-discrepancy, self-directed style, and emotion dysregulation. Int J Eat Disord. (2020) 53:1918–27. doi: 10.1002/eat.23389
PubMed Abstract | CrossRef Full Text | Google Scholar
27. Juarascio AS, Schumacher LM, Shaw J, Forman EM, Herbert JD. Acceptance-based treatment and quality of life among patients with an eating disorder. J Context Behav Sci. (2015) 4:42–7. doi: 10.1016/j.jcbs.2014.11.002
PubMed Abstract | CrossRef Full Text | Google Scholar
29. Lavender JM, Wonderlich SA, Peterson CB, Crosby RD, Engel SG, Mitchell JE, et al. Dimensions of emotion dysregulation in bulimia nervosa. Eur Eat Disord Rev. (2014) 22:212–6. doi: 10.1002/erv.2288
PubMed Abstract | CrossRef Full Text | Google Scholar
30. MacDonald DE, McFarlane TL, Dionne MM, David L, Olmsted MP. Rapid response to intensive treatment for bulimia nervosa and purging disorder: A randomized controlled trial of a CBT intervention to facilitate early behavior change. J Consult Clin Psychol. (2017) 85:896. doi: 10.1037/ccp0000221
PubMed Abstract | CrossRef Full Text | Google Scholar
31. MacDonald DE, Trottier K, Olmsted MP. Rapid improvements in emotion regulation predict intensive treatment outcome for patients with bulimia nervosa and purging disorder. Int J Eat Disord. (2017) 50:1152–61. doi: 10.1002/eat.22766
PubMed Abstract | CrossRef Full Text | Google Scholar
32. Michael ML, Juarascio A. Differences in eating disorder symptoms and affect regulation for residential eating disorder patients with problematic substance use. Eating Weight Disord. (2020) 25:1805–11. doi: 10.1007/s40519-019-00789-3
PubMed Abstract | CrossRef Full Text | Google Scholar
33. Monell E, Clinton D, Birgegård A. Self-directed behaviors differentially explain associations between emotion dysregulation and eating disorder psychopathology in patients with or without objective binge-eating. J Eat Disord. (2020) 8:17. doi: 10.1186/s40337-020-00294-4
PubMed Abstract | CrossRef Full Text | Google Scholar
34. Nagata, T., Matsuyama, M., Kiriike, N., Iketani, T., Oshima, J. (2000). Stress coping strategy in Japanese patients with eating disorders: relationship with bulimic and impulsive behaviors. The Journal of Nervous and mental disease, 188(5), 280–286.
PubMed Abstract | Google Scholar
35. Pisetsky EM, Haynos AF, Lavender JM, Crow SJ, Peterson CB. Associations between emotion regulation difficulties, eating disorder symptoms, non-suicidal self-injury, and suicide attempts in a heterogeneous eating disorder sample. Compr Psychiatry. (2017) 73:143–50. doi: 10.1016/j.comppsych.2016.11.012
PubMed Abstract | CrossRef Full Text | Google Scholar
36. Racine SE, Wildes JE. Emotion dysregulation and symptoms of anorexia nervosa: the unique roles of lack of emotional awareness and impulse control difficulties when upset. Int J Eat Disord. (2013) 46:713–20. doi: 10.1002/eat.22145
PubMed Abstract | CrossRef Full Text | Google Scholar
37. Racine SE, Wildes JE. Dynamic longitudinal relations between emotion regulation difficulties and anorexia nervosa symptoms over the year following intensive treatment. J Consult Clin Psychol. (2015) 83:785. doi: 10.1037/ccp0000011
PubMed Abstract | CrossRef Full Text | Google Scholar
39. Southward MW, Christensen KA, Fettich KC, Weissman J, Berona J, Chen EY. Loneliness mediates the relationship between emotion dysregulation and bulimia nervosa/binge eating disorder psychopathology in a clinical sample. Eating Weight Disord. (2014) 19:509–13. doi: 10.1007/s40519-013-0083-2
PubMed Abstract | CrossRef Full Text | Google Scholar
40. Steinglass JE, Glasofer DR, Walsh E, Guzman G, Peterson CB, Walsh BT, et al. Targeting habits in anorexia nervosa: a proof-of-concept randomized trial. Psychol Med. (2018) 48:2584–91. doi: 10.1017/S003329171800020X
PubMed Abstract | CrossRef Full Text | Google Scholar
41. Svaldi J, Griepenstroh J, Tuschen-Caffier B, Ehring T. Emotion regulation deficits in eating disorders: a marker of eating pathology or general psychopathology?. Psychiatry Res. (2012) 197:103–11. doi: 10.1016/j.psychres.2011.11.009
PubMed Abstract | CrossRef Full Text | Google Scholar
42. Turan S, Özyurt G, Çatli G, Öztürk Y, Abaci A, Akay AP. Social cognition and emotion regulation may be impaired in adolescents with obesity independent of the presence of binge eating disorder: a two-center study. Psychiatry Clin Psychopharmacol. (2019) 29:887–94. doi: 10.1080/24750573.2019.1693727
CrossRef Full Text | Google Scholar
43. Wisting L, Johnson SU, Bulik CM, Andreassen OA, Rø Ø, Bang L. Psychometric properties of the Norwegian version of the Patient Health Questionnaire-9 (PHQ-9) in a large female sample of adults with and without eating disorders. BMC Psychiatry. (2021) 21:6. doi: 10.1186/s12888-020-03013-0
PubMed Abstract | CrossRef Full Text | Google Scholar
44. Wolz I, Agüera Z, Granero R, Jiménez-Murcia S, Gratz KL, Menchón JM, et al. Emotion regulation in disordered eating: psychometric properties of the difficulties in emotion regulation scale among spanish adults and its interrelations with personality and clinical severity. Front Psychol. (2015) 6:e00907. doi: 10.3389/fpsyg.2015.00907
PubMed Abstract | CrossRef Full Text | Google Scholar
45. Wyssen A, Lao J, Rodger H, Humbel N, Lennertz J, Schuck K, et al. Facial emotion recognition abilities in women experiencing eating disorders. Psychosom Med. (2019) 81:155–64. doi: 10.1097/PSY.0000000000000664
PubMed Abstract | CrossRef Full Text | Google Scholar
47. Dajon M, Sudres JL. Orthorexia and eating disorders: a specific profile? Orthorexie et troubles des conduites alimentaires: spécificité d’un profil?. Ann Méd Psychol. (2021). doi: 10.1016/j.amp.2021.02.010
CrossRef Full Text | Google Scholar
48. Lee EB, Smith BM, Twohig MP, Lensegrav-Benson T, Quakenbush-Roberts B. Assessment of the body image-acceptance and action questionnaire in a female residential eating disorder treatment facility. J Context Behav Sci. (2017) 6:21–8. doi: 10.1016/j.jcbs.2016.11.004
CrossRef Full Text | Google Scholar
49. Manwaring J, Hilbert A, Walden K, Bishop ER, Johnson C. Validation of the acceptance and action questionnaire for weight-related difficulties in an eating disorder population. J Context Behav Sci. (2018) 7:1–7. doi: 10.1016/j.jcbs.2017.09.004
CrossRef Full Text | Google Scholar
50. Walden K, Manwaring J, Blalock DV, Bishop E, Duffy A, Johnson C. Acceptance and psychological change at the higher levels of care: a naturalistic outcome study. Eat Disord. (2018) 26:311–25. doi: 10.1080/10640266.2017.1400862
PubMed Abstract | CrossRef Full Text | Google Scholar
51. Butryn ML, Juarascio A, Shaw J, Kerrigan SG, Clark V, O’Planick A, et al. Mindfulness and its relationship with eating disorders symptomatology in women receiving residential treatment. Eat Behav. (2013) 14:13–6. doi: 10.1016/j.eatbeh.2012.10.005
PubMed Abstract | CrossRef Full Text | Google Scholar
52. Legenbauer T, Vocks S, Rüddel H. Emotion recognition, emotional awareness and cognitive bias in individuals with bulimia nervosa. J Clin Psychol. (2008) 64:687–702. doi: 10.1002/jclp.20483
PubMed Abstract | CrossRef Full Text | Google Scholar
53. Bernatova T, Svetlak M. Emotional and interoceptive awareness and its relationship to restriction in young women with eating disorders and healthy controls: a cascade from emotional to behavioral dysregulation. Act Nerv Super. (2017) 59:78–86. doi: 10.1007/s41470-017-0006-z
CrossRef Full Text | Google Scholar
54. Dunne JP, Shindul-Rothschild J, White L, Lee CS, Wolfe BE. Mindfulness in persons with anorexia nervosa and the relationships between eating disorder symptomology, anxiety and pain. Eat Disord. (2021) 29:497–508. doi: 10.1080/10640266.2019.1688009
PubMed Abstract | CrossRef Full Text | Google Scholar
55. Torres S, Sales C, Guerra MP, Simões MP, Pinto M, Vieira FM. Emotion-focused cognitive behavioral therapy in comorbid obesity with binge eating disorder: A pilot study of feasibility and long-term outcomes. Front Psychol. (2020) 11:343. doi: 10.3389/fpsyg.2020.00343
PubMed Abstract | CrossRef Full Text | Google Scholar
56. Messer M, Anderson C, Linardon J. Self-compassion explains substantially more variance in eating disorder psychopathology and associated impairment than mindfulness. Body Image. (2021) 36:27–33. doi: 10.1016/j.bodyim.2020.10.002
PubMed Abstract | CrossRef Full Text | Google Scholar
57. Compare A, Callus E, Grossi E. Mindfulness trait, eating behaviours and body uneasiness: a case-control study of binge eating disorder. Eat Weight Disord. (2012) 17:e244–51.
PubMed Abstract | Google Scholar
58. Lattimore P, Mead BR, Irwin L, Grice L, Carson R, Malinowski P. ‘I can’t accept that feeling’: relationships between interoceptive awareness, mindfulness and eating disorder symptoms in females with, and at-risk of an eating disorder. Psychiatry Res. (2017) 247:163–71. doi: 10.1016/j.psychres.2016.11.022
PubMed Abstract | CrossRef Full Text | Google Scholar
59. Pepping CA, O’Donovan A, Zimmer-Gembeck MJ, Hanisch M. Individual differences in attachment and eating pathology: the mediating role of mindfulness. Pers Individ Dif. (2015) 75:24–9. doi: 10.1016/j.paid.2014.10.040
CrossRef Full Text | Google Scholar
60. Pinto-Gouveia J, Carvalho SA, Palmeira L, Castilho P, Duarte C, Ferreira C, et al. BEfree: a new psychological program for binge eating that integrates psychoeducation, mindfulness, and compassion. Clin Psychol Psychother. (2017) 24:1090–8. doi: 10.1002/cpp.2072
PubMed Abstract | CrossRef Full Text | Google Scholar
61. Espel-Huynh HM, Muratore AF, Virzi N, Brooks G, Zandberg LJ. Mediating role of experiential avoidance in the relationship between anxiety sensitivity and eating disorder psychopathology: a clinical replication. Eat Behav. (2019) 34:101308. doi: 10.1016/j.eatbeh.2019.101308
PubMed Abstract | CrossRef Full Text | Google Scholar
62. Scharff A, Ortiz SN, Forrest LN, Smith AR, Boswell JF. Post-traumatic stress disorder as a moderator of transdiagnostic, residential eating disorder treatment outcome trajectory. J Clin Psychol. (2021) 77:986–1003. doi: 10.1002/jclp.23106
PubMed Abstract | CrossRef Full Text | Google Scholar
63. Paterson G, Power K, Collin P, Greirson D, Yellowlees A, Park K. A mediational model of self-esteem and social problem-solving in anorexia nervosa. Eur Eat Disord Rev. (2011) 19:112–20. doi: 10.1002/erv.1021
PubMed Abstract | CrossRef Full Text | Google Scholar
64. Paterson G, Power K, Yellowlees A, Park K, Taylor L. The relationship between two-dimensional self-esteem and problem solving style in an anorexic inpatient sample. Eur Eat Disord Rev. (2007) 15:70–7. doi: 10.1002/erv.708
PubMed Abstract | CrossRef Full Text | Google Scholar
65. Sternheim L, Danner U, van Elburg A, Harrison A. Do anxiety, depression, and intolerance of uncertainty contribute to social problem solving in adult women with anorexia nervosa? Brain Behav. (2020) 10:e01588. doi: 10.1002/brb3.1588
PubMed Abstract | CrossRef Full Text | Google Scholar
66. Fitzsimmons EE, Bardone-Cone AM. Coping and social support as potential moderators of the relation between anxiety and eating disorder symptomatology. Eat Behav. (2011) 12:21–8. doi: 10.1016/j.eatbeh.2010.09.002
PubMed Abstract | CrossRef Full Text | Google Scholar
67. Marchiol F, Penolazzi B, Cavallero C, Luxardi GL. The role of alexithymia and coping strategies in eating disorders: a pilot study. Act Nerv Super. (2020) 62:69–77. doi: 10.1007/s41470-019-00066-9
CrossRef Full Text | Google Scholar
69. Svaldi J, Dorn C, Trentowska M. Effectiveness for interpersonal problem-solving is reduced in women with binge eating disorder. Eur Eat Disord Rev. (2011) 19:331–41. doi: 10.1002/erv.1050
PubMed Abstract | CrossRef Full Text | Google Scholar
70. Davies MM, Bekker MH, Roosen MA. The role of coping and general psychopathology in the prediction of treatment outcome in eating disorders. Eat Disord. (2011) 19:246–58. doi: 10.1080/10640266.2011.566147
PubMed Abstract | CrossRef Full Text | Google Scholar
72. Oldershaw A, DeJong H, Hambrook D, Broadbent H, Tchanturia K, Treasure J, et al. Emotional processing following recovery from anorexia nervosa. Eur Eat Disord Rev. (2012) 20:502–9. doi: 10.1002/erv.2153
PubMed Abstract | CrossRef Full Text | Google Scholar
73. Raykos BC, Byrne SM, Watson H. Confirmatory and exploratory factor analysis of the distress tolerance scale (DTS) in a clinical sample of eating disorder patients. Eat Behav. (2009) 10:215–9. doi: 10.1016/j.eatbeh.2009.07.001
PubMed Abstract | CrossRef Full Text | Google Scholar
74. Danner UN, Evers C, Stok FM, van Elburg AA, de Ridder DT. A double burden: Emotional eating and lack of cognitive reappraisal in eating disordered women. Eur Eat Disord Rev. (2012) 20:490–5. doi: 10.1002/erv.2184
PubMed Abstract | CrossRef Full Text | Google Scholar
75. Danner UN, Sternheim L, Evers C. The importance of distinguishing between the different eating disorders (sub) types when assessing emotion regulation strategies. Psychiatry Res. (2014) 215:727–32. doi: 10.1016/j.psychres.2014.01.005
PubMed Abstract | CrossRef Full Text | Google Scholar
76. Davies H, Swan N, Schmidt U, Tchanturia K. An experimental investigation of verbal expression of emotion in anorexia and bulimia nervosa. Eur Eat Disord Rev. (2012) 20:476–83. doi: 10.1002/erv.1157
PubMed Abstract | CrossRef Full Text | Google Scholar
77. Rothschild-Yakar L, Peled M, Enoch-Levy A, Gur E, Stein D. “Eating me up from inside”: a pilot study of mentalization of self and others and emotion regulation strategies among young women with eating disorders. Israel J Psychiatry. (2018) 55:35–43.
PubMed Abstract | Google Scholar
78. Wildes JE, Ringham RM, Marcus MD. Emotion avoidance in patients with anorexia nervosa: Initial test of a functional model. Int J Eat Disord. (2010) 43:398–404. doi: 10.1002/eat.20730
PubMed Abstract | CrossRef Full Text | Google Scholar
79. Waller G, Kyriacou Marcoulides O. Safety behaviours in eating disorders: factor structure and clinical validation of the Brief Safety Behaviours Scale. Eur Eat Disord Rev. (2013) 21:257–61. doi: 10.1002/erv.2208
PubMed Abstract | CrossRef Full Text | Google Scholar
80. Mason TB, Lavender JM, Wonderlich SA, Crosby RD, Joiner TE, Mitchell JE, et al. The role of interpersonal personality traits and reassurance seeking in eating disorder symptoms and depressive symptoms among women with bulimia nervosa. Compr Psychiatry. (2016) 68:165–71. doi: 10.1016/j.comppsych.2016.04.013
PubMed Abstract | CrossRef Full Text | Google Scholar
81. Thaler L, Brassard S, Booij L, Kahan E, McGregor K, Labbe A, et al. Methylation of the OXTR gene in women with anorexia nervosa: relationship to social behavior. Eur Eat Disord Rev. (2020) 28:79–86. doi: 10.1002/erv.2703
PubMed Abstract | CrossRef Full Text | Google Scholar
82. Cockell SJ, Geller J, Linden W. Decisional balance in anorexia nervosa: Capitalizing on ambivalence. Eur Eat Disord Rev. (2003) 11:75–89. doi: 10.1002/erv.493
CrossRef Full Text | Google Scholar
83. Delinsky SS, Thomas JJ, Germain SAS, Ellison Craigen K, Weigel TJ, Levendusky PG, et al. Motivation to change among residential treatment patients with an eating disorder: assessment of the multidimensionality of motivation and its relation to treatment outcome. Int J Eat Disord. (2011) 44:340–8. doi: 10.1002/eat.20809
PubMed Abstract | CrossRef Full Text | Google Scholar
84. Rothschild-Yakar L, Stein D, Goshen D, Shoval G, Yacobi A, Eger G, et al. Mentalizing self and other and affect regulation patterns in anorexia and depression. Front Psychol. (2019) 10:2223. doi: 10.3389/fpsyg.2019.02223
PubMed Abstract | CrossRef Full Text | Google Scholar
85. Tasca GA, Szadkowski L, Illing V, Trinneer A, Grenon R, Demidenko N, et al. Adult attachment, depression, and eating disorder symptoms: the mediating role of affect regulation strategies. Pers Individ Dif. (2009) 47:662–7. doi: 10.1016/j.paid.2009.06.006
CrossRef Full Text | Google Scholar
86. Sheffield A, Waller G, Emanuelli F, Murray J, Meyer C. Do schema processes mediate links between parenting and eating pathology?. Eur Eat Disord Rev. (2009) 17:290–300. doi: 10.1002/erv.922
PubMed Abstract | CrossRef Full Text | Google Scholar
88. Noetel M, Miskovic-Wheatley J, Crosby RD, Hay P, Madden S, Touyz S. A clinical profile of compulsive exercise in adolescent inpatients with anorexia nervosa. J Eat Disord. (2016) 4:1–10. doi: 10.1186/s40337-016-0090-6
PubMed Abstract | CrossRef Full Text | Google Scholar
89. Sauchelli S, Arcelus J, Granero R, Jiménez-Murcia S, Agüera Z, Pino-Gutiérrez D, et al. Dimensions of compulsive exercise across eating disorder diagnostic subtypes and the validation of the Spanish version of the compulsive exercise test. Front Psychol. (2016) 7:1852. doi: 10.3389/fpsyg.2016.01852
PubMed Abstract | CrossRef Full Text | Google Scholar
90. Bratland-Sanda S, Sundgot-Borgen J, Rø Ø, Rosenvinge JH, Hoffart A, Martinsen EW. Physical activity and exercise dependence during inpatient treatment of longstanding eating disorders: An exploratory study of excessive and non-excessive exercisers. Int J Eat Disord. (2010) 43:266–73. doi: 10.1002/eat.20769
PubMed Abstract | CrossRef Full Text | Google Scholar
91. Marzola E, Panepinto C, Delsedime N, Amianto F, Fassino S, Abbate-Daga G. A factor analysis of the meanings of anorexia nervosa: intrapsychic, relational, and avoidant dimensions and their clinical correlates. BMC Psychiatry. (2016) 16:1–9. doi: 10.1186/s12888-016-0894-6
PubMed Abstract | CrossRef Full Text | Google Scholar
92. Meyer C, Serpell L, Waller G, Murphy F, Treasure J, Leung N. Cognitive avoidance in the strategic processing of ego threats among eating-disordered patients. Int J Eat Disord. (2005) 38:30–6. doi: 10.1002/eat.20147
PubMed Abstract | CrossRef Full Text | Google Scholar
93. Merwin RM, Zucker NL, Timko CA. A pilot study of an acceptance-based separated family treatment for adolescent anorexia nervosa. Cogn Behav Pract. (2013) 20:485–500. doi: 10.1016/j.cbpra.2012.11.001
PubMed Abstract | CrossRef Full Text | Google Scholar
95. Rienecke RD, Blalock DV, Duffy A, Manwaring J, Le Grange D, Johnson C, et al. Posttraumatic stress disorder symptoms and trauma-informed care in higher levels of care for eating disorders. Int J Eat Disord. (2021) 54:627–32. doi: 10.1002/eat.23455
PubMed Abstract | CrossRef Full Text | Google Scholar
96. Baños RM, Cebolla A, Moragrega I, Van Strien T, Fernández-Aranda F, Agüera Z, et al. Relationship between eating styles and temperament in an Anorexia Nervosa, Healthy Control, and Morbid Obesity female sample. Appetite. (2014) 76:76–83. doi: 10.1016/j.appet.2014.01.012
PubMed Abstract | CrossRef Full Text | Google Scholar
97. Danner UN, Sanders N, Smeets PA, van Meer F, Adan RA, Hoek HW, et al. Neuropsychological weaknesses in anorexia nervosa: Set-shifting, central coherence, and decision making in currently ill and recovered women. Int J Eat Disord. (2012) 45:685–94. doi: 10.1002/eat.22007
PubMed Abstract | CrossRef Full Text | Google Scholar
99. Duffy ME, Rogers ML, Joiner TE, Bergen AW, Berrettini W, Bulik CM, et al. An investigation of indirect effects of personality features on anorexia nervosa severity through interoceptive dysfunction in individuals with lifetime anorexia nervosa diagnoses. Int J Eat Disord. (2019) 52:200–5. doi: 10.1002/eat.23008
PubMed Abstract | CrossRef Full Text | Google Scholar
100. Frank GK, DeGuzman MC, Shott ME, Laudenslager ML, Rossi B, Pryor T. Association of brain reward learning response with harm avoidance, weight gain, and hypothalamic effective connectivity in adolescent anorexia nervosa. JAMA Psychiatry. (2018) 75:1071–80. doi: 10.1001/jamapsychiatry.2018.2151
PubMed Abstract | CrossRef Full Text | Google Scholar
101. Levinson CA, Zerwas SC, Brosof LC, Thornton LM, Strober M, Pivarunas B, et al. Associations between dimensions of anorexia nervosa and obsessive-compulsive disorder: an examination of personality and psychological factors in patients with anorexia nervosa. Eur Eat Disord Rev. (2019) 27:161–72. doi: 10.1002/erv.2635
PubMed Abstract | CrossRef Full Text | Google Scholar
102. Del Pino-Gutiérrez A, Jiménez-Murcia S, Fernández-Aranda F, Agüera Z, Granero R, Hakansson A, et al. The relevance of personality traits in impulsivity-related disorders: from substance use disorders and gambling disorder to bulimia nervosa. J Behav Addict. (2017) 6:396–405. doi: 10.1556/2006.6.2017.051
PubMed Abstract | CrossRef Full Text | Google Scholar
103. Paganini C, Peterson G, Andrews K. The Mediating role of temperamental traits on the relationship between age of puberty and eating disorders: a mediating analysis through structural equation modelling of Australian eating disorder outpatients. J Genet Psychol. (2021) 1–15. doi: 10.1080/00221325.2021.1940822
PubMed Abstract | CrossRef Full Text | Google Scholar
104. Rotella F, Fioravanti G, Godini L, Mannucci E, Faravelli C, Ricca V. Temperament and emotional eating: a crucial relationship in eating disorders. Psychiatry Res. (2015) 225:452–7. doi: 10.1016/j.psychres.2014.11.068
PubMed Abstract | CrossRef Full Text | Google Scholar
105. Van Riel L, Van den Berg E, Polak M, Geerts M, Peen J, Ingenhoven T, et al. Personality functioning in obesity and binge eating disorder: combining a psychodynamic and trait perspective. J Psychiatr Pract. (2020) 26:472–84. doi: 10.1097/PRA.0000000000000513
PubMed Abstract | CrossRef Full Text | Google Scholar
106. Wierenga CE, Bischoff-Grethe A, Berner LA, Simmons AN, Bailer U, Paulus MP, et al. Increased anticipatory brain response to pleasant touch in women remitted from bulimia nervosa. Transl Psychiatry. (2020) 10:1–14. doi: 10.1038/s41398-020-00916-0
PubMed Abstract | CrossRef Full Text | Google Scholar
107. Solmi M, Collantoni E, Meneguzzo P, Degortes D, Tenconi E, Favaro A. Network analysis of specific psychopathology and psychiatric symptoms in patients with eating disorders. Int J Eat Disord. (2018) 51:680–92. doi: 10.1002/eat.22884
PubMed Abstract | CrossRef Full Text | Google Scholar
108. Marzola E, Fassino S, Migliaretti G, Abbate-Daga G, Kaye WH. Development and validation of the Premorbid Childhood Traits Questionnaire (PCT-Q) in eating disorders. Eating Weight Disord. (2019) 24:815–23. doi: 10.1007/s40519-019-00748-y
PubMed Abstract | CrossRef Full Text | Google Scholar
109. Verschueren M, Luyckx K, Kaufman EA, Vansteenkiste M, Moons P, Sleuwaegen E, et al. Identity Processes and Statuses in Patients with and without Eating Disorders. Eur Eat Disord Rev. (2017) 25:26–35. doi: 10.1002/erv.2487
PubMed Abstract | CrossRef Full Text | Google Scholar
110. Wang SB, Lydecker JA, Grilo CM. Rumination in patients with binge-eating disorder and obesity: Associations with eating-disorder psychopathology and weight-bias internalization. Eur Eat Disord Rev. (2017) 25:98–103. doi: 10.1002/erv.2499
PubMed Abstract | CrossRef Full Text | Google Scholar
111. Sagiv E, Gvion Y. A multi factorial model of self-harm behaviors in Anorexia-nervosa and Bulimia-nervosa. Compr Psychiatry. (2020) 96:152142. doi: 10.1016/j.comppsych.2019.152142
PubMed Abstract | CrossRef Full Text | Google Scholar
112. Wang SB, Borders A. The unique effects of angry and depressive rumination on eating-disorder psychopathology and the mediating role of impulsivity. Eat Behav. (2018) 29:41–7. doi: 10.1016/j.eatbeh.2018.02.004
PubMed Abstract | CrossRef Full Text | Google Scholar
113. Thew GR, Gregory JD, Roberts K, Rimes KA. The phenomenology of self-critical thinking in people with depression, eating disorders, and in healthy individuals. Psychol Psychother Theor Res Pract. (2017) 90:751–69. doi: 10.1111/papt.12137
PubMed Abstract | CrossRef Full Text | Google Scholar
114. Seidel M, Petermann J, Diestel S, Ritschel F, Boehm I, King JA, et al. A naturalistic examination of negative affect and disorder-related rumination in anorexia nervosa. Eur Child Adolesc Psychiatry. (2016) 25:1207–16. doi: 10.1007/s00787-016-0844-3
PubMed Abstract | CrossRef Full Text | Google Scholar
115. Overton A, Selway S, Strongman K, Houston M. Eating disorders-The regulation of positive as well as negative emotion experience. J Clin Psychol Med Settings. (2005) 12:39–56. doi: 10.1007/s10880-005-0911-2
CrossRef Full Text | Google Scholar
116. Cardi V, Corfield F, Leppanen J, Rhind C, Deriziotis S, Hadjimichalis A, et al. Emotional processing of infants displays in eating disorders. PLoS ONE. (2014) 9:e113191. doi: 10.1371/journal.pone.0113191
PubMed Abstract | CrossRef Full Text | Google Scholar
117. Davies H, Schmidt U, Stahl D, Tchanturia K. Evoked facial emotional expression and emotional experience in people with anorexia nervosa. Int J Eat Disord. (2011) 44:531–9. doi: 10.1002/eat.20852
PubMed Abstract | CrossRef Full Text | Google Scholar
118. Dapelo MM, Hart S, Hale C, Morris R, Lynch TR, Tchanturia K. Facial expression of positive emotions in individuals with eating disorders. Psychiatry Res. (2015) 230:70–7. doi: 10.1016/j.psychres.2015.08.019
PubMed Abstract | CrossRef Full Text | Google Scholar
119. Lang K, Larsson EE, Mavromara L, Simic M, Treasure J, Tchanturia K. Diminished facial emotion expression and associated clinical characteristics in Anorexia Nervosa. Psychiatry Res. (2016) 236:165–72. doi: 10.1016/j.psychres.2015.12.004
PubMed Abstract | CrossRef Full Text | Google Scholar
120. Leppanen J, Cardi V, Ng KW, Paloyelis Y, Stein D, Tchanturia K, et al. Effects of intranasal oxytocin on the interpretation and expression of emotions in anorexia nervosa. J Neuroendocrinol. (2017) 29. doi: 10.1111/jne.12458
PubMed Abstract | CrossRef Full Text | Google Scholar
121. Krug I, Bulik CM, Vall-Llovera ON, Granero R, Agüera Z, Villarejo C, et al. Anger expression in eating disorders: clinical, psychopathological and personality correlates. Psychiatry Res. (2008) 161:195–205. doi: 10.1016/j.psychres.2007.10.003
PubMed Abstract | CrossRef Full Text | Google Scholar
122. Fassino S, Leombruni P, Pierò A, Abbate-Daga G, Rovera GG. Mood, eating attitudes, and anger in obese women with and without binge eating disorder. J Psychosom Res. (2003) 54:559–66. doi: 10.1016/S0022-3999(02)00462-2
PubMed Abstract | CrossRef Full Text | Google Scholar
123. Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. (2004) 26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94
PubMed Abstract | CrossRef Full Text | Google Scholar
124. Platt JJ, Spivack G. Manual for the Means-Ends Problem-Solving Procedure (MEPS): A Measure of Interpersonal Cognitive Problem-Solving Skill. Philadelphia, PA: Community Mental Health, Mental Retardation Center, Department of Mental Health Sciences, Hahnemann Medical College and Hospital (1975).
Google Scholar
125. D’Zurilla TJ, Nezu AM, Maydeu-Olivares A. Social Problem-Solving Inventory-Revised. North Tonawanda, NY: Multi-Health Systems (2002).
Google Scholar
126. Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol. (2003) 85:348–62. doi: 10.1037/0022-3514.85.2.348
PubMed Abstract | CrossRef Full Text | Google Scholar
127. Garcia D, Lester N, Cloninger KM, Robert Cloninger C. Temperament and character inventory (TCI) BT – encyclopedia of personality and individual differences. In: Zeigler-Hill V, Shackelford TK, editors. Cham: Springer International Publishing (2017). p. 1–3.
Google Scholar
128. Treynor W, Gonzalez R, Nolen-Hoeksema S. Rumination reconsidered: a psychometric analysis. Cognit Ther Res. (2003) 27:247–59. doi: 10.1023/A:1023910315561
CrossRef Full Text | Google Scholar
131. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. (2010) 36:1–48. doi: 10.18637/jss.v036.i03
CrossRef Full Text | Google Scholar
133. Palmieri S, Mansueto G, Scaini S, Caselli G, Sapuppo W, Spada MM, et al. Repetitive negative thinking and eating disorders: a meta-analysis of the role of worry and rumination. J Clin Med. (2021) 10:2448. doi: 10.3390/jcm10112448
PubMed Abstract | CrossRef Full Text | Google Scholar
135. Sala M, Brosof LC, Levinson C. Repetitive negative thinking predicts eating disorder behaviors: a pilot ecological momentary assessment study in a treatment seeking eating disorder sample. Behav Res Ther. (2019) 112:12–7. doi: 10.1016/j.brat.2018.11.005
PubMed Abstract | CrossRef Full Text | Google Scholar
136. Smith KE, Mason TB, Reilly EE, Hazzard VM, Borg SL, Dvorak R, et al. Examining prospective mediational relationships between momentary rumination, negative affect, and binge eating using ecological momentary assessment. J Affect Disord Reports. (2021) 5:100138. doi: 10.1016/j.jadr.2021.100138
PubMed Abstract | CrossRef Full Text | Google Scholar
137. Svaldi J, Werle D, Naumann E, Eichler E, Berking M. Prospective associations of negative mood and emotion regulation in the occurrence of binge eating in binge eating disorder. J Psychiatr Res. (2019) 115:61–8. doi: 10.1016/j.jpsychires.2019.05.005
PubMed Abstract | CrossRef Full Text | Google Scholar
138. Cowdrey FA, Park RJ. Assessing rumination in eating disorders: principal component analysis of a minimally modified ruminative response scale. Eat Behav. (2011) 12:321–4. doi: 10.1016/j.eatbeh.2011.08.001
PubMed Abstract | CrossRef Full Text | Google Scholar
139. Fürtjes S, Seidel M, King JA, Biemann R, Roessner V, Ehrlich S. Rumination in anorexia nervosa: cognitive-affective and neuroendocrinological aspects. Behav Res Ther. (2018) 111:92–8. doi: 10.1016/j.brat.2018.10.001
PubMed Abstract | CrossRef Full Text | Google Scholar
140. Ridout SJ, Ridout KK, Kole J, Fitzgerald KL, Donaldson AA, Alverson B. Comparison of eating disorder characteristics and depression comorbidity in adolescent males and females: an observational study. Psychiatry Res. (2021) 296:113650. doi: 10.1016/j.psychres.2020.113650
PubMed Abstract | CrossRef Full Text | Google Scholar
142. Svaldi J, Naumann E. Effects of rumination and acceptance on body dissatisfaction in binge eating disorder. European Eating Disorders Review. (2014) 22:338–45. doi: 10.1002/erv.2312
PubMed Abstract | CrossRef Full Text | Google Scholar
143. Smith KE, Juarascio A. From ecological momentary assessment (EMA) to ecological momentary intervention (EMI): past and future directions for ambulatory assessment and interventions in eating disorders. Curr Psychiatry Rep. (2019) 21:53. doi: 10.1007/s11920-019-1046-8
PubMed Abstract | CrossRef Full Text | Google Scholar
145. Racine SE, Horvath SA. Emotion dysregulation across the spectrum of pathological eating: comparisons among women with binge eating, overeating, and loss of control eating. Eat Disord. (2018) 26:13–25. doi: 10.1080/10640266.2018.1418381
PubMed Abstract | CrossRef Full Text | Google Scholar
146. Mallorqui-Bague N, Vintro-Alcaraz C, Sanchez I, Riesco N, Aguera Z, Granero R, et al. Emotion regulation as a transdiagnostic feature among eating disorders: cross-sectional and longitudinal approach. Eur Eat Disord Rev. (2018) 26:53–61. doi: 10.1002/erv.2570
PubMed Abstract | CrossRef Full Text | Google Scholar
147. Juarascio AS, Manasse SM, Schumacher L, Espel H, Forman EM. Developing an acceptance-based behavioral treatment for binge eating disorder: rationale and challenges. Cogn Behav Pract. (2017) 24:1–13. doi: 10.1016/j.cbpra.2015.12.005
PubMed Abstract | CrossRef Full Text | Google Scholar
148. Hayes SC, Strosahl K, Wilson KG, Bissett RT, Pistorello J, Toarmino D, et al. Measuring experiential avoidance: a preliminary test of a working model. Psychol Rec. (2004) 54:553–78. doi: 10.1007/BF03395492
CrossRef Full Text | Google Scholar
150. Lavender JM, Wonderlich SA, Engel SG, Gordon KH, Kaye WH, Mitchell JE. Dimensions of emotion dysregulation in anorexia nervosa and bulimia nervosa: a conceptual review of the empirical literature. Clin Psychol Rev. (2015) 40:111–22. doi: 10.1016/j.cpr.2015.05.010
PubMed Abstract | CrossRef Full Text | Google Scholar
151. Giorgio JM, Sanflippo J, Kleiman E, Reilly D, Bender RE, Wagner CA, et al. An experiential avoidance conceptualization of depressive rumination: three tests of the model. Behav Res Ther. (2010) 48:1021–31. doi: 10.1016/j.brat.2010.07.004
PubMed Abstract | CrossRef Full Text | Google Scholar
152. Brockmeyer T, Holtforth MG, Bents H, Kämmerer A, Herzog W, Friederich HC. Starvation and emotion regulation in anorexia nervosa. Compr Psychiatry. (2012) 53:496–501. doi: 10.1016/j.comppsych.2011.09.003
PubMed Abstract | CrossRef Full Text | Google Scholar
153. Haynos AF, Fruzzetti AE. Anorexia Nervosa as a disorder of emotion dysregulation: evidence and treatment implications. Clin Psychol Sci Pract. (2011) 18:183–202. doi: 10.1111/j.1468-2850.2011.01250.x
CrossRef Full Text | Google Scholar
154. Henderson ZB, Fox JRE, Trayner P, Wittkowski A. Emotional development in eating disorders: a qualitative metasynthesis. Clin Psychol Psychother. (2019) 26:440–57. doi: 10.1002/cpp.2365
PubMed Abstract | CrossRef Full Text | Google Scholar
155. Oldershaw A, Startup H, Lavender T. Anorexia Nervosa and a lost emotional self: a psychological formulation of the development, maintenance, and treatment of Anorexia Nervosa. Front Psychol. (2019) 10:1–22. doi: 10.3389/fpsyg.2019.00219
PubMed Abstract | CrossRef Full Text | Google Scholar
156. Schmidt U, Treasure J. Anorexia nervosa: valued and visible. A cognitive-interpersonal maintenance model and its implications for research and practice. Br J Clin Psychol. (2006) 45:343–66. doi: 10.1348/014466505X53902
PubMed Abstract | CrossRef Full Text | Google Scholar
157. Normann N, van Emmerik AAP, Morina N. The efficacy of metacognitive therapy for anxiety and depression: a meta-analytic review. Depress Anxiety. (2014) 31:402–11. doi: 10.1002/da.22273
PubMed Abstract | CrossRef Full Text | Google Scholar
158. Spinhoven P, Klein N, Kennis M, Cramer A, Siegle G, Cuijpers P, et al. The effects of cognitive-behavior therapy for depression on repetitive negative thinking: a meta-analysis. Behav Res Ther. (2018) 106:71–85. doi: 10.1016/j.brat.2018.04.002
PubMed Abstract | CrossRef Full Text | Google Scholar
159. Watkins ER, Mullan E, Wingrove J, Rimes K, Steiner H, Bathurst N, et al. Rumination-focused cognitive-behavioural therapy for residual depression: phase II randomised controlled trial. Br J Psychiatry. (2011) 199:317–22. doi: 10.1192/bjp.bp.110.090282
PubMed Abstract | CrossRef Full Text | Google Scholar
160. Robertson S, Strodl E. Metacognitive therapy for binge eating disorder: a case series study. Clin Psychol. (2020) 24:143–54. doi: 10.1111/cp.12213
CrossRef Full Text | Google Scholar
161. Papageorgiou C. Metacognitive theory, therapy and techniques: introduction to the special issue. Cognit Ther Res. (2015) 39:1–3. doi: 10.1007/s10608-014-9649-1
CrossRef Full Text | Google Scholar
162. Wells A, Fisher P, Myers S, Wheatley J, Patel T, Brewin CR. Metacognitive therapy in recurrent and persistent depression: a multiple-baseline study of a new treatment. Cognit Ther Res. (2009) 33:291–300. doi: 10.1007/s10608-007-9178-2
CrossRef Full Text | Google Scholar
163. Manlick CF, Cochran SV, Koon J. Acceptance and commitment therapy for eating disorders: rationale and literature review. J Contemp Psychother. (2013) 43:115–22. doi: 10.1007/s10879-012-9223-7
CrossRef Full Text | Google Scholar
164. Berman MI, Boutelle KN, Crow SJ. A case series investigating acceptance and commitment therapy as a treatment for previously treated, unremitted patients with anorexia nervosa. Eur Eat Disord Rev. (2009) 17:426–34. doi: 10.1002/erv.962
PubMed Abstract | CrossRef Full Text | Google Scholar
165. Hill ML, Masuda A, Melcher H, Morgan JR, Twohig MP. Acceptance and commitment therapy for women diagnosed with binge eating disorder: a case-series study. Cogn Behav Pract. (2015) 22:367–78. doi: 10.1016/j.cbpra.2014.02.005
CrossRef Full Text | Google Scholar
167. Fogelkvist M, Gustafsson SA, Kjellin L, Parling T. Acceptance and commitment therapy to reduce eating disorder symptoms and body image problems in patients with residual eating disorder symptoms: a randomized controlled trial. Body Image. (2020) 32:155–66. doi: 10.1016/j.bodyim.2020.01.002
PubMed Abstract | CrossRef Full Text | Google Scholar
168. Griffiths C, Williamson H, Zucchelli F, Paraskeva N, Moss T. A systematic review of the effectiveness of acceptance and commitment therapy (ACT) for body image dissatisfaction and weight self-stigma in adults. J Contemp Psychother. (2018) 48:189–204. doi: 10.1007/s10879-018-9384-0
PubMed Abstract | CrossRef Full Text | Google Scholar
170. Gillikin LM, Manasse SM, Seager van Dyk I. An examination of emotion regulation as a mechanism underlying eating disorder pathology in lesbian, gay, and bisexual individuals. Eat Behav. (2021) 41:101508. doi: 10.1016/j.eatbeh.2021.101508
PubMed Abstract | CrossRef Full Text | Google Scholar