Binge-eating disorder was first described in 1959 by the American psychiatrist Albert Stunkard to illustrate the characteristics of a subgroup of patients with obesity and recurrent episodes of excessive and uncontrolled eating; a behavior he called binge eating.
However, its existence as a distinct eating disorder was ignored until the second half of the 1980s, when some studies on the prevalence of bulimia nervosa in the population discovered a large subgroup of individuals who did not use compensatory behaviors after binge episodes. In the same period, it was observed that about a quarter of individuals who required obesity treatment reported recurrent binge-eating episodes but did not suffer from bulimia nervosa.
In 1994, the American Psychiatric Association (APA) included binge-eating disorder (BED) as an example of an eating disorder not otherwise specified and, in Appendix B of the Statistical and Diagnostic Manual of Mental Disorders (DSM-IV), provided a list of diagnostic criteria for further study. Subsequent studies confirmed that BED has distinctive clinical characteristics compared to bulimia nervosa and obesity by supporting the validity and clinical utility of a BED diagnosis. However, the disorder was recognized by DSM-5 as a distinct diagnostic category only in 2003.
In the last 15 years, more than 2000 articles on BED have been published in international scientific journals, and today we have extensive knowledge of its main clinical features. However, studies have also shown the limited effect of available treatments on weight loss when BED is associated with obesity.
Recently some authors have proposed the ketogenic diet as a potential treatment to promote both the control of binge episodes and weight loss, but the evidence to support this indication is scarce. In addition, as I will explain in this post, ketogenic diets can maintain and aggravate binge episodes in people with BED and obesity.
BED and obesity
Although also present in some normal-weight individuals, BED is more frequent in those with obesity. The fact that binge-eating episodes are not followed by regular use of compensatory behaviors and often occur in a context where there is a general tendency to overeat explains its association with obesitỳ. Among people seeking obesity treatment, between 1.4% and 9% meet the DSM diagnostic criteria of BED. However, binge-eating episodes have been reported in the same population, ranging from 9% to 29%.
BED and ketogenic diets
Ketogenic diets are dietary patterns with high fat (≈60%), low carbohydrate (≈10%), and moderate protein levels (≈30%). If individuals adhere to this dietary pattern, nutritional ketosis occurs that results in an increased lipolysis, metabolic costs of gluconeogenesis and the thermal effect of proteins, and reduced lipogenesis. In some people, ketogenesis also appears to result in a slight short-term decrease in appetite and hunger and increased satiety. Such effects have led some clinicians to prescribe the ketogenic diet to people with obesity and BED. This recommendation was based on the observation that people with BED often report an inability to tolerate hunger, satiety disorders (e.g., “they never feel full”), and food craving, and cite these physical experiences as the most significant impediment to achieving eating control and weight loss.
The effects of the ketogenic diet in patients with binge-eating episodes and obesity have been evaluated only in two case studies of three and five patients who reported binge eating and food addiction. While describing a potentially beneficial effect of the ketogenic diet on eating behavior and short-term weight loss, both studies have important methodological limitations. First, the evaluations, having been made only in the short term, do not allow conclusions about the long-term effects of these diets on eating behavior and weight. Then, both studies evaluated the presence of binge eating with the Binge Eating Scale (BES) questionnaire, which has many false positives, and with the Yale Food Addiction Scale (YFAS), which assesses the controversial presence of so-called “food addiction.” Finally, the absence of control cases precludes any conclusion about the role of ketogenic diets compared to other dietary interventions.
Dysfunctional dietary restraint and binge eating
People with BED and obesity report with high frequency the adoption of a dysfunctional dietary restriction characterized by the intermittent adoption of extreme and strict dietary rules to lose weight and change their body shape, dictating what, when, and how much they are “allowed” or “not allowed” to eat. Examples of dietary rules characterizing a dysfunctional diet include:
“Avoid carbohydrates completely because they make you fat” (as recommended by ketogenic diets).
“Don’t eat anything after 18:00.”
“Eat less than 1,000 calories a day.”
“Eat only one a meal a day.”
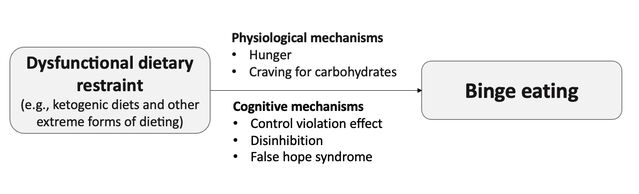
Dysfunctional dietary restriction is implicated in maintaining binge episodes through the main mechanisms described in the following paragraphs (see Figure 1).
Ketogenic Diet Essential Reads
Dysfunctional dietary restraint maintains binge eating.
Source: Dalle Grave, M.D.
Physiological mechanisms
Hunger. Although the early stages of some dysfunctional diets (e.g., ketogenic diets) may be associated with a decrease in appetite, in a more or less long time, hunger almost always takes over, and it is associated with an increase in concerns about food and eating. When people succumb to hunger, they often overeat and binge on the foods they have avoided.
Craving for carbohydrates. A long-term high-protein diet increases plasma levels of amino acids that compete with tryptophan for transport in the brain (e.g., leucine, isoleucine, and valine), thereby decreasing tryptophan flow through the blood-brain barrier and brain serotonin levels with possible deflection of mood and increased carbohydrate intake when they are introduced with the diet.
Cognitive mechanisms
Control violation effect. It is a cognitive behavioral reaction to the almost inevitable breakdown of “extreme dietary rules” that characterize dysfunctional dietary restriction. Indeed, people often attribute breaking dietary rules to a lack of willpower or personal value and not to the fact that their dietary rules are extreme and rigid. This interpretation often determines the development of cognitive dissonance (e.g., “I am worth if I don’t binge—I’m not worth if I binge”), which produces thoughts and behaviors aimed at reducing the dissonance itself (e.g., “I will never be able to control my eating; I am destined to binge all my life; therefore it is better that I eat what I want and abandon any attempt to control eating”). In this way, the person can continue to binge without feeling guilty.
Disinhibition. People who adopt extreme and strict dietary rules use self-control and willpower to control their diet. This rigid cognitive control makes them vulnerable to disinhibition when something else hinders the exercise of self-control (e.g., alcohol, events, and associated mood changes),
False hope syndrome. Some people with BED and obesity paradoxically persist in repeated attempts at weight loss with dysfunctional diets, despite previous failures. Initial weight loss often provides powerful positive reinforcement, even if followed by failure, because feelings of control and optimism often accompany it. Unrealistic expectations regarding the ease, speed, likely degree of weight loss, and potential benefits that will be achieved from weight loss tend to overwhelm knowledge derived from previous failures. The false hope of those who follow dysfunctional diets reflects the desire to believe that you can get what you want: false hopes develop because people want to believe in them.
Healthy and flexible diet and binge-eating disorder
A healthy and flexible diet, characterized by adopting healthy and flexible dietary guidelines, including the intake of a wide variety of foods, appears to be the optimal strategy to recommend to patients with BED and obesity. This recommendation is supported by a study in which it was found that rigid eating control is associated with higher scores of eating disinhibition, higher body mass index (BMI), and more frequent and severe episodes of binge eating. On the contrary, flexible eating control was associated with lower levels of eating disinhibition, lower BMI, less frequent and severe episodes of binge eating, lower reported energy intake, and a higher probability of success in weight management during treatment.
Conclusions
Currently, we do not have empirical data supporting ketogenic diets’ usefulness and safety in treating patients with BED associated with obesity. In contrast, dysfunctional diets (such as the ketogenic diets that eliminate many foods) play an important role in maintaining and aggravating binge episodes through numerous physiological and cognitive mechanisms.
In conclusion, like other dysfunctional diets, ketogenic diets are “contraindicated” in treating binge-eating disorder and other eating disorders.

