Arcelus, J., Mitchell, A. J., Wales, J. & Nielsen, S. Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 36 studies. Arch. Gen. Psychiat. 68, 724–731 (2011).
Google Scholar
Smink, F. R. E., van Hoeken, D. & Hoek, H. W. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr. Psychiat. Rep. 14, 406–414 (2012).
Fichter, M. M., Quadflieg, N. & Hedlund, S. Long-term course of binge eating disorder and bulimia nervosa: relevance for nosology and diagnostic criteria. Int. J. Eat. Disord. 41, 577–586 (2008).
Google Scholar
Suokas, J. T. et al. Mortality in eating disorders: a follow-up study of adult eating disorder patients treated in tertiary care, 1995–2010. Psychiat. Res. 210, 1101–1106 (2013).
Roberts, M. E., Tchanturia, K., Stahl, D., Southgate, L. & Treasure, J. A systematic review and meta-analysis of set-shifting ability in eating disorders. Psychol. Med. 37, 1075–1084 (2007).
Google Scholar
Rosval, L. et al. Impulsivity in women with eating disorders: problem of response inhibition, planning, or attention? Int. J. Eat. Disord. 39, 590–593 (2006).
Google Scholar
Tchanturia, K. et al. An investigation of decision making in anorexia nervosa using the Iowa Gambling Task and skin conductance measurements. J. Int. Neuropsychol. Soc. 13, 635–641 (2007).
Google Scholar
Keel, P. K., Mitchell, J. E., Miller, K. B., Davis, T. L. & Crow, S. J. Social adjustment over 10 years following diagnosis with bulimia nervosa. Int. J. Eat. Disord. 27, 21–28 (2000).
Google Scholar
de la Rie, S., Noordenbos, G., Donker, M. & van Furth, E. The patient’s view on quality of life and eating disorders. Int. J. Eat. Disord. 40, 13–20 (2007).
Google Scholar
Klump, K. L., Bulik, C. M., Kaye, W. H., Treasure, J. & Tyson, E. Academy for eating disorders position paper: eating disorders are serious mental illnesses. Int. J. Eat. Disord. 42, 97–103 (2009).
Google Scholar
Tyler, I., Wiseman, M. C., Crawford, R. I. & Birmingham, C. L. Cutaneous manifestations of eating disorders. J. Cutan. Med. Surg. 6, 345–353 (2002).
Google Scholar
Lifante-Oliva, C., López-Jornet, P., Camacho-Alonso, F. & Esteve-Salinas, J. Study of oral changes in patients with eating disorders. Int. J. Dent. Hyg. 6, 119–122 (2008).
Google Scholar
Powers, P. S. Osteoporosis and eating disorders. J. Pediatr. Adolesc. Gynecol. 12, 51–57 (1999).
Google Scholar
Awazu, M., Matsuoka, S., Kamimaki, T., Watanabe, H. & Matsuo, N. Absent circadian variation of blood pressure in patients with anorexia nervosa. J. Pediatr. 136, 524–527 (2000).
Google Scholar
Muuss, R. E. Adolescent eating disorder: anorexia nervosa. Adolescence 20, 525–536 (1985).
Google Scholar
Braude, M. R. et al. Acute medical stabilisation of adults with anorexia nervosa: experience of a defined interdisciplinary model of care. Intern. Med. J. 50, 77–85 (2020).
Google Scholar
Mitchell, J. E., Pomeroy, C. & Huber, M. A clinician’s guide to the eating disorders medicine cabinet. Int. J. Eat. Disord. 7, 211–223 (1988).
Swenne, I. Poor catch-up growth in late adolescent boys with eating disorders, weight loss and stunting of growth. Eur. Eat. Disord. Rev. 21, 395–398 (2013).
Google Scholar
Tith, R. M. et al. Association of bulimia nervosa with long-term risk of cardiovascular disease and mortality among women. JAMA Psychiat. 77, 44–51 (2020).
Tabler, J., Utz, R. L., Smith, K. R., Hanson, H. A. & Geist, C. Variation in reproductive outcomes of women with histories of bulimia nervosa, anorexia nervosa, or eating disorder not otherwise specified relative to the general population and closest-aged sisters. Int. J. Eat. Disord. 51, 102–111 (2018).
Google Scholar
Porcelli, P., Leandro, G. & De Carne, M. Functional gastrointestinal disorders and eating disorders: relevance of the association in clinical management. Scand. J. Gastroenterol. 33, 577–582 (1998).
Google Scholar
Coffino, J. A., Udo, T. & Grilo, C. M. Rates of help-seeking in US adults with lifetime DSM-5 eating disorders: prevalence across diagnoses and differences by sex and ethnicity/race. Mayo Clin. Proc. 94, 1415–1426 (2019).
Google Scholar
van den Berg, E. et al. Meta-analysis on the efficacy of psychological treatments for anorexia nervosa. Eur. Eat. Disord. Rev. 27, 331–351 (2019).
Google Scholar
McFarlane, T., Olmsted, M. P. & Trottier, K. Timing and prediction of relapse in a transdiagnostic eating disorder sample. Int. J. Eat. Disord. 41, 587–593 (2008).
Google Scholar
Streatfeild, J. et al. Social and economic cost of eating disorders in the United States: evidence to inform policy action. Int. J. Eat. Disord. 54, 851–868 (2021).
Google Scholar
Fried, E. I. Lack of theory building and testing impedes progress in the factor and network literature. Psychol. Inq. 31, 271–288 (2020).
Hudson, J. I., Hiripi, E., Pope, H. G. & Kessler, R. C. The prevalence and correlates of eating disorders in the national comorbidity survey replication. Biol. Psychiat. 61, 348–358 (2007).
Google Scholar
Godart, N. T., Flament, M. F., Perdereau, F. & Jeammet, P. Comorbidity between eating disorders and anxiety disorders: a review. Int. J. Eat. Disord. 32, 253–270 (2002).
Google Scholar
Kaye, W. H., Bulik, C. M., Thornton, L., Barbarich, N. & Masters, K. Comorbidity of anxiety disorders with anorexia and bulimia nervosa. Am. J. Psychiat. 161, 2215–2221 (2004).
Google Scholar
Kerr-Gaffney, J., Harrison, A. & Tchanturia, K. Social anxiety in the eating disorders: a systematic review and meta-analysis. Psychol. Med. 48, 2477–2491 (2018).
Google Scholar
Mandelli, L., Draghetti, S., Albert, U., De Ronchi, D. & Atti, A.-R. Rates of comorbid obsessive-compulsive disorder in eating disorders: a meta-analysis of the literature. J. Affect. Disord. 277, 927–939 (2020).
Google Scholar
Ruffolo, J. S., Phillips, K. A., Menard, W., Fay, C. & Weisberg, R. B. Comorbidity of body dysmorphic disorder and eating disorders: severity of psychopathology and body image disturbance. Int. J. Eat. Disord. 39, 11–19 (2006).
Google Scholar
Mitchell, K. S., Mazzeo, S. E., Schlesinger, M. R., Brewerton, T. D. & Smith, B. N. Comorbidity of partial and subthreshold PTSD among men and women with eating disorders in the National Comorbidity Survey-Replication study. Int. J. Eat. Disord. 45, 307–315 (2012).
Google Scholar
DeSocio, J. E. Challenges in diagnosis and treatment of comorbid eating disorders and mood disorders. Perspect. Psychiat. Care 55, 494–500 (2019).
McElroy, S. L., Kotwal, R., Keck, P. E. & Akiskal, H. S. Comorbidity of bipolar and eating disorders: distinct or related disorders with shared dysregulations? J. Affect. Disord. 86, 107–127 (2005).
Google Scholar
McElroy, S. L. et al. Prevalence and correlates of eating disorders in 875 patients with bipolar disorder. J. Affect. Disord. 128, 191–198 (2011).
Google Scholar
Bleck, J. R., DeBate, R. D. & Olivardia, R. The comorbidity of ADHD and eating disorders in a nationally representative sample. J. Behav. Health Serv. Res. 42, 437–451 (2015).
Google Scholar
Brewerton, T. D. & Duncan, A. E. Associations between attention deficit hyperactivity disorder and eating disorders by gender: results from the National Comorbidity Survey Replication. Eur. Eat. Disord. Rev. 24, 536–540 (2016).
Google Scholar
Bahji, A. et al. Prevalence of substance use disorder comorbidity among individuals with eating disorders: a systematic review and meta-analysis. Psychiat. Res. 273, 58–66 (2019).
Cassin, S. & Vonranson, K. Personality and eating disorders: a decade in review. Clin. Psychol. Rev. 25, 895–916 (2005).
Google Scholar
Sansone, R. A., Levitt, J. L. & Sansone, L. A. The prevalence of personality disorders among those with eating disorders. Eat. Disord. 13, 7–21 (2004).
O’Brien, K. M. & Vincent, N. K. Psychiatric comorbidity in anorexia and bulimia nervosa: nature, prevalence, and causal relationships. Clin. Psychol. Rev. 23, 57–74 (2003).
Google Scholar
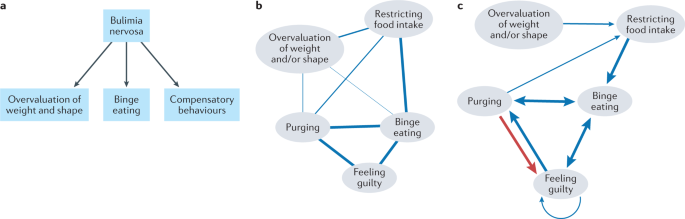
Fairburn, C. G., Cooper, Z. & Shafran, R. Cognitive behaviour therapy for eating disorders: a ‘transdiagnostic’ theory and treatment. Behav. Res. Ther. 41, 509–528 (2003).
Google Scholar
Lock, J. & le Grange, D. Family-based treatment of eating disorders. Int. J. Eat. Disord. 37, S64–S67 (2005).
Google Scholar
Herzog, D. B., Nussbaum, K. M. & Marmor, A. K. Comorbidity and outcome in eating disorders. Psychiat. Clin. North. Am. 19, 843–859 (1996).
Carr, M. M. & Grilo, C. M. Examining heterogeneity of binge-eating disorder using latent class analysis. J. Psychiat. Res. 130, 194–200 (2020).
Google Scholar
Riesco, N. et al. Other specified feeding or eating disorders (OSFED): clinical heterogeneity and cognitive-behavioral therapy outcome. Eur. Psychiat. 54, 109–116 (2018).
Sysko, R., Hildebrandt, T., Wilson, G. T., Wilfley, D. E. & Agras, W. S. Heterogeneity moderates treatment response among patients with binge eating disorder. J. Consult. Clin. Psychol. 78, 681–690 (2010).
Google Scholar
Fairweather-Schmidt, A. K. & Wade, T. D. DSM-5 eating disorders and other specified eating and feeding disorders: is there a meaningful differentiation? Int. J. Eat. Disord. 47, 524–533 (2014).
Google Scholar
Thomas, J. J., Vartanian, L. R. & Brownell, K. D. The relationship between eating disorder not otherwise specified (EDNOS) and officially recognized eating disorders: meta-analysis and implications for DSM. Psychol. Bull. 135, 407–433 (2009).
Google Scholar
Galmiche, M., Déchelotte, P., Lambert, G. & Tavolacci, M. P. Prevalence of eating disorders over the 2000–2018 period: a systematic literature review. Am. J. Clin. Nutr. 109, 1402–1413 (2019).
Google Scholar
Fairburn, C. G. & Cooper, Z. Eating disorders, DSM-5 and clinical reality. Br. J. Psychiat. 198, 8–10 (2011).
Keel, P. K., Brown, T. A., Holm-Denoma, J. & Bodell, L. P. Comparison of DSM-IV versus proposed DSM-5 diagnostic criteria for eating disorders: reduction of eating disorder not otherwise specified and validity. Int. J. Eat. Disord. 44, 553–560 (2011).
Google Scholar
Frank, G. K. W., Shott, M. E. & DeGuzman, M. C. The neurobiology of eating disorders. Child. Adolesc. Psychiat. Clin. N. Am. 28, 629–640 (2019).
Brooks, S. J., Rask-Andersen, M., Benedict, C. & Schiöth, H. B. A debate on current eating disorder diagnoses in light of neurobiological findings: is it time for a spectrum model? BMC Psychiat. 12, 76 (2012).
Forbush, K. T. et al. Understanding eating disorders within internalizing psychopathology: a novel transdiagnostic, hierarchical-dimensional model. Compr. Psychiat. 79, 40–52 (2017).
Google Scholar
Levinson, C. A., Vanzhula, I. & Brosof, L. C. Longitudinal and personalized networks of eating disorder cognitions and behaviors: targets for precision intervention a proof of concept study. Int. J. Eat. Disord. 51, 1233–1243 (2018).
Google Scholar
Wilson, G. T., Grilo, C. M. & Vitousek, K. M. Psychological treatment of eating disorders. Am. Psychol. 62, 199–216 (2007).
Google Scholar
Keel, P. K. & Mitchell, J. E. Outcome in bulimia nervosa. Am. J. Psychiat. 154, 313–321 (1997).
Google Scholar
Keel, P. K., Dorer, D. J., Franko, D. L., Jackson, S. C. & Herzog, D. B. Postremission predictors of relapse in women with eating disorders. Am. J. Psychiat. 162, 2263–2268 (2005).
Google Scholar
Carter, J. C. et al. A prospective study of predictors of relapse in anorexia nervosa: implications for relapse prevention. Psychiat. Res. 200, 518–523 (2012).
Eddy, K. T. et al. Diagnostic crossover in anorexia nervosa and bulimia nervosa: implications for DSM-V. Am. J. Psychiat. 165, 245–250 (2008).
Google Scholar
Plessow, F. & Eddy, K. T. in Encyclopedia of Feeding and Eating Disorders (ed. Wade, T.) (Springer, 2016).
Castellini, G. et al. Diagnostic crossover and outcome predictors in eating disorders according to DSM-IV and DSM-V proposed criteria: a 6-year follow-up study. Psychosom. Med. 73, 270–279 (2011).
Google Scholar
Tozzi, F. et al. Symptom fluctuation in eating disorders: correlates of diagnostic crossover. Am. J. Psychiat. 162, 732–740 (2005).
Google Scholar
Stice, E., Marti, C. N., Shaw, H. & Jaconis, M. An 8-year longitudinal study of the natural history of threshold, subthreshold, and partial eating disorders from a community sample of adolescents. J. Abnorm. Psychol. 118, 587–597 (2009).
Google Scholar
Bulik, C. M., Sullivan, P. F., Fear, J. & Pickering, A. Predictors of the development of bulimia nervosa in women with anorexia nervosa. J. Nerv. Ment. Dis. 185, 704–707 (1997).
Google Scholar
Strober, M., Freeman, R. & Morrell, W. The long-term course of severe anorexia nervosa in adolescents: survival analysis of recovery, relapse, and outcome predictors over 10–15 years in a prospective study. Int. J. Eat. Disord. 22, 339–360 (1997).
Google Scholar
Forbush, K. T. et al. A new approach to eating-disorder classification: using empirical methods to delineate diagnostic dimensions and inform care. Int. J. Eat. Disord. 51, 710–721 (2018).
Google Scholar
Milos, G., Spindler, A., Schnyder, U. & Fairburn, C. G. Instability of eating disorder diagnoses: prospective study. Br. J. Psychiat. 187, 573–578 (2005).
American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders 5th edn (American Psychiatric Association, 2013).
Borsboom, D. & Cramer, A. O. J. Network analysis: an integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 9, 91–121 (2013).
Google Scholar
Bringmann, L. F. & Eronen, M. I. Don’t blame the model: reconsidering the network approach to psychopathology. Psychol. Rev. 125, 606–615 (2018).
Google Scholar
Borsboom, D. A network theory of mental disorders. World Psychiat. 16, 5–13 (2017).
Jones, P. J. & Robinaugh, D. R. An answer to “so what?” implications of network theory for research and practice. FOCUS 19, 204–210 (2021).
Google Scholar
Epskamp, S., Borsboom, D. & Fried, E. I. Estimating psychological networks and their accuracy: a tutorial paper. Behav. Res. Methods 50, 195–212 (2018).
Google Scholar
Guyon, H., Falissard, B. & Kop, J.-L. Modeling psychological attributes in psychology — an epistemological discussion: network analysis vs. latent variables. Front. Psychol. 8, 798 (2017).
Google Scholar
Costantini, G. et al. State of the aRt personality research: a tutorial on network analysis of personality data in R. J. Res. Personal. 54, 13–29 (2015).
Cramer, A. O. J. et al. Dimensions of normal personality as networks in search of equilibrium: you can’t like parties if you don’t like people. Eur. J. Personal. 26, 414–431 (2012).
van Bork, R. et al. Latent variable models and networks: statistical equivalence and testability. Multivar. Behav. Res. 56, 175–198 (2021).
Burger, J. et al. Bridging the gap between complexity science and clinical practice by formalizing idiographic theories: a computational model of functional analysis. BMC Med. 18, 99 (2020).
Google Scholar
Levinson, C. A., Vanzhula, I. A., Brosof, L. C. & Forbush, K. Network analysis as an alternative approach to conceptualizing eating disorders: implications for research and treatment. Curr. Psychiat. Rep. 20, 67 (2018).
Cramer, A. O. J., Waldorp, L. J., van der Maas, H. L. J. & Borsboom, D. Comorbidity: a network perspective. Behav. Brain Sci. 33, 137–150 (2010).
Google Scholar
Keel, P. K. & Brown, T. A. Update on course and outcome in eating disorders. Int. J. Eat. Disord. 43, 195–204 (2010).
Google Scholar
Roy-Byrne, P. P. et al. Lifetime panic–depression comorbidity in the National Comorbidity Survey: association with symptoms, impairment, course and help-seeking. Br. J. Psychiat. 176, 229–235 (2000).
Nock, M. K., Hwang, I., Sampson, N. A. & Kessler, R. C. Mental disorders, comorbidity and suicidal behavior: results from the national comorbidity survey replication. Mol. Psychiat. 15, 868–876 (2010).
Kessler, R. C. et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiat. 62, 593–602 (2005).
Google Scholar
Jones, P. J., Ma, R. & McNally, R. J. Bridge centrality: a network approach to understanding comorbidity. Multivar. Behav. Res. 56, 353–367 (2021).
Plana-Ripoll, O. et al. Exploring comorbidity within mental disorders among a Danish national population. JAMA Psychiat. 76, 259–270 (2019).
van Loo, H. M., Romeijn, J.-W., de Jonge, P. & Schoevers, R. A. Psychiatric comorbidity and causal disease models. Prev. Med. 57, 748–752 (2013).
Google Scholar
Lilienfeld, S. O. The Research Domain Criteria (RDoC): an analysis of methodological and conceptual challenges. Behav. Res. Ther. 62, 129–139 (2014).
Google Scholar
Pallister, E. & Waller, G. Anxiety in the eating disorders: understanding the overlap. Clin. Psychol. Rev. 28, 366–386 (2008).
Google Scholar
Bulik, C. M., Sullivan, P. F., Fear, J. L. & Joyce, P. R. Eating disorders and antecedent anxiety disorders: a controlled study. Acta Psychiatr. Scand. 96, 101–107 (1997).
Google Scholar
Levinson, C. A. & Rodebaugh, T. L. Social anxiety and eating disorder comorbidity: the role of negative social evaluation fears. Eat. Behav. 13, 27–35 (2012).
Google Scholar
Konstantellou, A., Campbell, M., Eisler, I., Simic, M. & Treasure, J. Testing a cognitive model of generalized anxiety disorder in the eating disorders. J. Anxiety Disord. 25, 864–869 (2011).
Google Scholar
Vanzhula, I. A., Calebs, B., Fewell, L. & Levinson, C. A. Illness pathways between eating disorder and post-traumatic stress disorder symptoms: understanding comorbidity with network analysis. Eur. Eat. Disord. Rev. 27, 147–160 (2019).
Google Scholar
Levinson, C. A. et al. Social anxiety and eating disorder comorbidity and underlying vulnerabilities: using network analysis to conceptualize comorbidity. Int. J. Eat. Disord. 51, 693–709 (2018).
Google Scholar
Meier, M. et al. Obsessive–compulsive symptoms in eating disorders: a network investigation. Int. J. Eat. Disord. 53, 362–371 (2020).
Google Scholar
Vanzhula, I. A., Kinkel-Ram, S. S. & Levinson, C. A. Perfectionism and difficulty controlling thoughts bridge eating disorder and obsessive-compulsive disorder symptoms: a network analysis. J. Affect. Disord. 283, 302–309 (2021).
Google Scholar
Forrest, L. N., Sarfan, L. D., Ortiz, S. N., Brown, T. A. & Smith, A. R. Bridging eating disorder symptoms and trait anxiety in patients with eating disorders: a network approach. Int. J. Eat. Disord. 52, 701–711 (2019).
Google Scholar
Levinson, C. A. et al. The core symptoms of bulimia nervosa, anxiety, and depression: a network analysis. J. Abnorm. Psychol. 126, 340–354 (2017).
Google Scholar
Ralph-Nearman, C., Williams, B. M., Ortiz, A. M. L., Smith, A. R. & Levinson, C. A. Pinpointing core and pathway symptoms among sleep disturbance, anxiety, worry, and eating disorder symptoms in anorexia nervosa and atypical anorexia nervosa. J. Affect. Disord. 294, 24–32 (2021).
Google Scholar
Sahlan, R. N. et al. Disordered eating, self-esteem, and depression symptoms in Iranian adolescents and young adults: a network analysis. Int. J. Eat. Disord. 54, 132–147 (2021).
Google Scholar
Cusack, C. E., Christian, C., Drake, J. E. & Levinson, C. A. A network analysis of eating disorder symptoms and co-occurring alcohol misuse among heterosexual and sexual minority college women. Addict. Behav. 118, 106867 (2021).
Google Scholar
Levinson, C. A. et al. Eating disorder symptoms and core eating disorder fears decrease during online imaginal exposure therapy for eating disorders. J. Affect. Disord. 276, 585–591 (2020).
Google Scholar
Beltz, A. M., Moser, J. S., Zhu, D. C., Burt, S. A. & Klump, K. L. Using person-specific neural networks to characterize heterogeneity in eating disorders: illustrative links between emotional eating and ovarian hormones. Int. J. Eat. Disord. 51, 730–740 (2018).
Google Scholar
Levinson, C. A., Vanzhula, I. A., Smith, T. W. & Stice, E. Group and longitudinal intra-individual networks of eating disorder symptoms in adolescents and young adults at-risk for an eating disorder. Behav. Res. Ther. 135, 103731 (2020).
Google Scholar
Fichter, M. M. & Quadflieg, N. How precisely can psychotherapists predict the long-term outcome of anorexia nervosa and bulimia nervosa at the end of inpatient treatment? Int. J. Eat. Disord. 54, 535–544 (2021).
Google Scholar
Nakash, O. & Saguy, T. Social identities of clients and therapists during the mental health intake predict diagnostic accuracy. Soc. Psychol. Personal. Sci. 6, 710–717 (2015).
Featherston, R., Downie, L. E., Vogel, A. P. & Galvin, K. L. Decision making biases in the allied health professions: a systematic scoping review. PLoS ONE 15, e0240716 (2020).
Google Scholar
Molenaar, P. C. M. A manifesto on psychology as idiographic science: bringing the person back into scientific psychology, this time forever. Meas. Interdiscip. Res. Perspect. 2, 201–218 (2004).
Fried, E. I. & Cramer, A. O. J. Moving forward: challenges and directions for psychopathological network theory and methodology. Perspect. Psychol. Sci. 12, 999–1020 (2017).
Google Scholar
Epskamp, S. et al. Personalized network modeling in psychopathology: the importance of contemporaneous and temporal connections. Clin. Psychol. Sci. 6, 416–427 (2018).
Google Scholar
Epskamp, S., Waldorp, L. J., Mõttus, R. & Borsboom, D. The Gaussian graphical model in cross-sectional and time-series data. Multivar. Behav. Res. 53, 453–480 (2018).
Fisher, A. J. et al. Exploring the idiographic dynamics of mood and anxiety via network analysis. J. Abnorm. Psychol. 126, 1044–1056 (2017).
Google Scholar
Bringmann, L. F. et al. A network approach to psychopathology: new insights into clinical longitudinal data. PLoS ONE 8, e60188 (2013).
Google Scholar
Piccirillo, M. L. & Rodebaugh, T. L. Foundations of idiographic methods in psychology and applications for psychotherapy. Clin. Psychol. Rev. 71, 90–100 (2019).
Google Scholar
Piccirillo, M. L., Beck, E. D. & Rodebaugh, T. L. A clinician’s primer for idiographic research: considerations and recommendations. Behav. Ther. 50, 938–951 (2019).
Google Scholar
Bringmann, L. F. Person-specific networks in psychopathology: past, present, and future. Curr. Opin. Psychol. 41, 59–64 (2021).
Google Scholar
Robinaugh, D. J., Hoekstra, R. H. A., Toner, E. R. & Borsboom, D. The network approach to psychopathology: a review of the literature 2008–2018 and an agenda for future research. Psychol. Med. 50, 353–366 (2020).
Google Scholar
Burger, J. et al. A clinical PREMISE for personalized models: towards a formal integration of case formulations and statistical networks. Preprint at PsyArXiv https://doi.org/10.31234/osf.io/bdrs7 (2021).
Google Scholar
Beck, A. T. Cognitive therapy: past, present, and future. J. Consult. Clin. Psychol. 61, 194–198 (1993).
Google Scholar
Linehan, M. M. in Cognitive-Behavioral Treatment Of Borderline Personality Disorder 558 (Guilford, 1993).
Hayes, S. C., Strosahl, K. D., Bunting, K., Twohig, M. & Wilson, K. G. What is acceptance and commitment therapy? In A Practical Guide to Acceptance and Commitment Therapy (eds Hayes, S. C. & Strosahl, K. D.) 3–29 (Springer, 2004).
Wright, J. H. Cognitive behavior therapy: basic principles and recent advances. Focus 4, 173–178 (2006).
Beck, J. S. & Beck, J. S. Cognitive Behavior Therapy: Basics and Beyond (Guilford, 2011).
Wenzel, A. Modification of core beliefs in cognitive therapy. In Standard and Innovative Strategies in Cognitive Behavior Therapy (ed. de Oliveira, I. R.) 17–34 (InTech, 2012).
Beck, A. T. The current state of cognitive therapy: a 40-year retrospective. Arch. Gen. Psychiat. 62, 953–959 (2005).
Google Scholar
Hopko, D. R., Lejuez, C. W., Ruggiero, K. J. & Eifert, G. H. Contemporary behavioral activation treatments for depression: procedures, principles, and progress. Clin. Psychol. Rev. 23, 699–717 (2003).
Google Scholar
Fried, E. I. et al. Mental disorders as networks of problems: a review of recent insights. Soc. Psychiat. Psychiatr. Epidemiol. 52, 1–10 (2017).
Halmi, K. A. Salient components of a comprehensive service for eating disorders. World Psychiatr. Assoc. 8, 150–155 (2009).
Anderson, L. K. et al. Treating eating disorders at higher levels of care: overview and challenges. Curr. Psychiat. Rep. 19, 48 (2017).
Walfish, S., McAlister, B., O’Donnell, P. & Lambert, M. J. An investigation of self-assessment bias in mental health providers. Psychol. Rep. 110, 639–644 (2012).
Google Scholar
Fernandez, K. C., Fisher, A. J. & Chi, C. Development and initial implementation of the Dynamic Assessment Treatment Algorithm (DATA). PLoS ONE 12, e0178806 (2017).
Google Scholar
Garb, H. N. Clinical judgment and decision making. Annu. Rev. Clin. Psychol. 1, 67–89 (2005).
Google Scholar
Dawes, R. M., Faust, D. & Meehl, P. E. Clinical versus actuarial judgment. Science 243, 1668–1674 (1989).
Google Scholar
Kraus, D. R. et al. Predicting therapist effectiveness from their own practice-based evidence. J. Consult. Clin. Psychol. 84, 473–483 (2016).
Google Scholar
Constantino, M. J., Boswell, J. F., Coyne, A. E., Swales, T. P. & Kraus, D. R. Effect of matching therapists to patients vs assignment as usual on adult psychotherapy outcomes: a randomized clinical trial. JAMA Psychiat. 78, 960–969 (2021).
Bulik, C. M., Berkman, N. D., Brownley, K. A., Sedway, J. A. & Lohr, K. N. Anorexia nervosa treatment: a systematic review of randomized controlled trials. Int. J. Eat. Disord. 40, 310–320 (2007).
Google Scholar
Kaye, W. H. & Bulik, C. M. Treatment of patients with anorexia nervosa in the US — a crisis in care. JAMA Psychiat. 78, 591 (2021).
Fairburn, C. G. Evidence-based treatment of anorexia nervosa. Int. J. Eat. Disord. 37, S26–S30 (2005).
Google Scholar
Levinson, C. A. et al. Using individual networks to identify treatment targets for eating disorder treatment: a proof-of-concept study and initial data. J. Eat. Disord. 9, 147 (2021).
Google Scholar
Frumkin, M. R., Piccirillo, M. L., Beck, E. D., Grossman, J. T. & Rodebaugh, T. L. Feasibility and utility of idiographic models in the clinic: a pilot study. Psychother. Res. J. Soc. Psychother. Res. 31, 520–534 (2021).
Galatzer-Levy, I. R. & Bryant, R. A. 636,120 ways to have posttraumatic stress disorder. Perspect. Psychol. Sci. 8, 651–662 (2013).
Google Scholar
Kotov, R. et al. The Hierarchical Taxonomy of Psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J. Abnorm. Psychol. 126, 454–477 (2017).
Google Scholar
Conway, C. C. & Krueger, R. F. Rethinking the diagnosis of mental disorders: data-driven psychological dimensions, not categories, as a framework for mental-health research, treatment, and training. Curr. Dir. Psychol. Sci. 30, 151–158 (2021).
Rubel, J. A., Fisher, A. J., Husen, K. & Lutz, W. Translating person-specific network models into personalized treatments: development and demonstration of the dynamic assessment treatment algorithm for individual networks (DATA-IN). Psychother. Psychosom. 87, 249–251 (2018).
Google Scholar
Bringmann, L. F. et al. What do centrality measures measure in psychological networks? J. Abnorm. Psychol. 128, 892–903 (2019).
Google Scholar
Levinson, C. A. et al. Longitudinal group and individual networks of eating disorder symptoms in individuals diagnosed with an eating disorder. J. Psychopathol. Clin. Sci. 131, 58–72 (2022).
Google Scholar
Spiller, T. R. et al. On the validity of the centrality hypothesis in cross-sectional between-subject networks of psychopathology. BMC Med. 18, 297 (2020).
Google Scholar
Levinson, C. A. et al. Personalized networks of eating disorder symptoms predicting eating disorder outcomes and remission. Int. J. Eat. Disord. 53, 2086–2094 (2020).
Google Scholar
Klintwall, L., Bellander, M. & Cervin, M. Perceived causal problem networks: reliability, central problems, and clinical utility for depression. Assessment https://doi.org/10.1177/10731911211039281 (2021).
Lunansky, G. et al. Intervening on psychopathology networks: evaluating intervention targets through simulations. Methods https://doi.org/10.1016/j.ymeth.2021.11.006 (2021).
Mansueto, A. C., Wiers, R. W., van Weert, J. C. M., Schouten, B. C. & Epskamp, S. Investigating the feasibility of idiographic network models. Psychol. Methods https://doi.org/10.1037/met0000466 (2022).
Google Scholar
Quax, R., Apolloni, A. & Sloot, P. M. A. The diminishing role of hubs in dynamical processes on complex networks. J. R. Soc. Interface 10, 20130568 (2013).
Google Scholar
Wright, A. G. C. et al. The hierarchical structure of DSM-5 pathological personality traits. J. Abnorm. Psychol. 121, 951–957 (2012).
Google Scholar
Godart, N. T. et al. Anxiety disorders in subjects seeking treatment for eating disorders: a DSM-IV controlled study. Psychiat. Res. 117, 245–258 (2003).
Godart, N. T., Flament, M. F., Lecrubier, Y. & Jeammet, P. Anxiety disorders in anorexia nervosa and bulimia nervosa: co-morbidity and chronology of appearance. Eur. Psychiat. J. Assoc. Eur. Psychiat. 15, 38–45 (2000).
Swinbourne, J. M. & Touyz, S. W. The co-morbidity of eating disorders and anxiety disorders: a review. Eur. Eat. Disord. Rev. 15, 253–274 (2007).
Google Scholar
Shah, R. & Zanarini, M. C. Comorbidity of borderline personality disorder. Psychiat. Clin. North. Am. 41, 583–593 (2018).
McNally, R. J. Can network analysis transform psychopathology? Behav. Res. Ther. 86, 95–104 (2016).
Google Scholar
Contreras, A., Nieto, I., Valiente, C., Espinosa, R. & Vazquez, C. The study of psychopathology from the network analysis perspective: a systematic review. Psychother. Psychosom. 88, 71–83 (2019).
Google Scholar
von Klipstein, L., Borsboom, D. & Arntz, A. The exploratory value of cross-sectional partial correlation networks: predicting relationships between change trajectories in borderline personality disorder. PLoS ONE 16, e0254496 (2021).
Boschloo, L., van Borkulo, C. D., Borsboom, D. & Schoevers, R. A. A prospective study on how symptoms in a network predict the onset of depression. Psychother. Psychosom. 85, 183–184 (2016).
Google Scholar
van Borkulo, C. et al. Association of symptom network structure with the course of depression. JAMA Psychiat. 72, 1219–1226 (2015).
Fried, E. I. Moving forward: how depression heterogeneity hinders progress in treatment and research. Expert Rev. Neurother. 17, 423–425 (2017).
Google Scholar