
.
*Content warning: disordered eating*
Writer and editor Emma Gunavardhana – host of the eponymous health and beauty podcast The Emma Guns Show – has long battled with her body image.
In pursuing one solution to remedy the issue, she uncovered the problem at the heart of her struggles: a turbulent relationship with food that turned out to be binge eating disorder.
Here, she writes for Women’s Health about her journey of discovery with binge eating disorder – and the binge eating disorder recovery strategy that worked for her.
You’ll find expert advice on binge eating disorder (including what is binge eating disorder and binge eating disorder treatment options) after Emma’s story.
But remember, if you’re struggling, help is available via BEAT, the UK’s Eating Disorder charity.
When I hit puberty, aged 12, my body changed drastically; I went from child-like to very curvy almost overnight. The change I found hardest to accept was my large breasts.
My first bra, a 32D, was thick-strapped, full-cupped and all about giving me support. I gained weight during puberty, yet my breasts – the things I had to heave up and strap down every day – were the greatest source of my unhappiness.
Still, it was another three decades before I decided to do something about it. Aged 41, I opted for breast reduction surgery in the hope I would finally feel comfortable in my own skin.
I reasoned that without these large 38F breasts – that were a struggle to dress, always making me look matronly – I’d look slim. Or at least not fat.
But looking at myself after the operation was… anticlimactic. That something as drastic as cosmetic surgery, requiring a general anaesthetic and six weeks’ recovery, didn’t fix how I felt made me face the underlying issue: my unhealthy – frankly, disordered – relationship with food.
How Binge Eating Disorder Developed for Me
The groundwork was laid between the ages of 12 and 17. When my breasts and weight changed significantly with the onset of puberty, I also developed acne, facial and excess body hair and was extremely lethargic.
My mother took me to the doctor aged 12, but I was told I was just ‘eating too much’ and it took another five years until a specialist diagnosed me with polycystic ovary syndrome (PCOS).
Five years is a very long time to feel disconnected from – and uncomfortable in – your body and it was during this time that I began to develop some extremely unhealthy eating habits.
Comfort eating and bingeing only added to the weight gain caused by my out-of-balance hormones. In the following years, I’d lose weight, only to put it back on again – and by the time I reached my forties, I was exhausted from decades of yo-yo-ing.
Part of me wanted to tap out and just embrace my body for how it looked. But, deep down, I realised that if I accepted my body as overweight, I had to accept I wasn’t going to do anything about the disordered eating that had got me there.
The effect on my self-esteem was huge; I believed that, because of my size, ‘normal’ things – boyfriends, parties and success – happened to other people. I didn’t feel I deserved them because if I couldn’t stand the sight of myself, how could anyone else? It’s no wonder I’d pinned my hopes on surgery.
This Surprising Binge Eating Treatment Worked for Me
Diet and exercise had never solved my issues so, after speaking to a friend who had overcome her own disordered eating by reading Kathryn Hansen’s Brain Over Binge, I got stuck in.
I recognised that I had a binge-eating disorder similar to bulimia, minus the purging. It was more than a little confronting. I’d avoided admitting that I ate too much for a long time. (And, trust me, you don’t spend the majority of your life carrying excess weight without people mentioning it might be prudent that you eat less.)
Camellia Publishing, LLC Brain over Binge: Why I Was Bulimic, Why Conventional Therapy Didn’t Work, and How I Recovered for Good
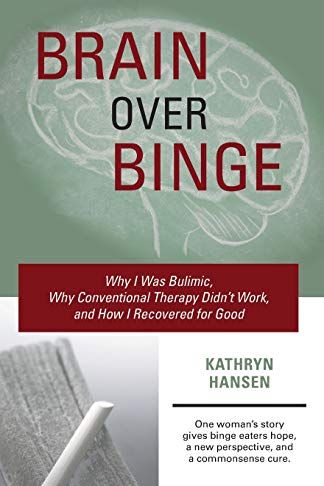
The book allowed me to see the urges to binge for what they were and it radically changed both how and what I ate. There was no dieting, just a new link in the chain between feeling the urge and attempting to satisfy it, which meant I stopped where I would have previously continued to eat.
I started to appreciate the nutritional value of each meal, and if I ever found myself feeling like I wanted more, I could rationalise that there was no way I could physically be hungry, which meant I could then dismiss the urge accordingly.
Five months later, in February 2020, I’d lost 30lb and it hadn’t felt like an effort. A year on, the weight has stayed off and my new way of eating has become…normal.
I occasionally feel the urge for a blow-out, but I recognise the difference between indulgence, like a takeaway, and a binge. I feel like I’ve found the key to unlock the door that kept me trapped in a cycle of food guilt and shame.
Where I’m at With my Binge Eating Disorder Recovery
While the process has been life-changing, I’m keen to emphasise that this is me in recovery, as opposed to me recovered, with my disordered eating being solved and my body image issues tied up in a neat bow.
Most days are straightforward, but occasionally there are times that I need to dig a bit deeper to prevent myself from retreating back into the cycle that restrained my life for so long. I’m not going to tell you that confronting your demons is easy – but the struggle is probably worth it.
A book was my catalyst to finally being honest with myself and understanding the role I was playing in my own discomfort, which allowed me to make meaningful and long-term lifestyle changes. It may be a GP visit or therapy sessions for you.
The journey might seem intimidating but, for me, it was the best thing I ever did – and it could be for you, too.
Binge Eating Disorder: The Expert View
Dr Lorna Richards is a consultant psychiatrist specialising in adult eating disorders at the Priory’s Life Works Rehabilitation Centre in Woking
What is binge eating disorder (BED) and how can you spot it?
It’s a serious mental illness and one of the most common eating disorders, accounting for 22% of known cases. The key symptom is eating – in a way that feels out of control or compulsive – an objectively excessive amount of food in a short period of time.
These episodes are very distressing and lead sufferers to have feelings of guilt, shame and disgust. For this reason, people often keep their difficulties secret and find it hard to ask for help.
What causes BED?
The disorder can develop for a number of reasons. Those with low self-esteem are most vulnerable, while dietary restriction can trigger or exacerbate it. It can also develop as a way of managing or numbing difficult emotions and become a habitual way of coping.
Many sufferers become overweight, which can significantly negatively impact their physical and mental health. They may develop depression and anxiety, and relationships and work can also be affected.
Where can someone seek support for BED?
If anyone feels that their relationship with food, eating or weight has become problematic – either because of their behaviour or how preoccupied they have become with thinking about these issues – they should seek help from their GP.
Treatment for BED consists of specialist psychological therapy, while antidepressant medication can also be helpful.
Having support to eat regularly in order to meet nutritional needs and manage emotions, alongside developing an understanding of how the problem has developed in the first place, will aid recovery.
If you’re worried about your own or someone else’s relationship with food, contact Beat, the UK’s eating disorder charity, on 0808 801 0677

