1 Introduction
Healthy food consumption has emerged as a significant trend in contemporary society, reflecting people’s pursuit of health and longevity. It is crucial for maintaining a healthy lifestyle (Luo et al., 2021; Kennedy et al., 2023). The vulnerability of food systems cannot curb malnutrition and stunting in children, making it more difficult for people to pursue healthy food (Haq et al., 2023). Currently, unhealthy dietary habits are closely linked to chronic conditions such as heart disease, hypertension, diabetes, and increased mortality (Solbak et al., 2017). The Interpretation of Report on Cardiovascular Health and Diseases in China 2022 notes that cardiovascular diseases such as hypertension and diabetes have become the leading cause of death for both urban and rural residents in China, with 48% in rural and 45.86% in urban areas. It seriously affects people’s health status and has become a significant public health problem (Liu Y. et al., 2021). Furthermore, the dietary structure of most Chinese individuals does not align with the recommended Chinese food pyramid structure (Xu et al., 2015). Food consumption patterns of households are determined by their socio-economic status. Underconsumption of healthy foods is a severe problem for policymakers and nutritionists worldwide, especially in developing countries (Lian et al., 2023). Therefore, enhancing the structure of healthy food consumption presents a critical challenge in China. Likewise, as a good starting point for developing sustainable lifestyles, it is increasingly attracting global attention, and growing evidence highlights the actual and potential value of healthy food consumption in improving public health and promoting food security.
A close interconnection and mutual influence exists between consumer behavior and healthy food consumption (Eyinade et al., 2021). As public health awareness grows, more consumers focus on their dietary habits and overall health status (Ghufran et al., 2022). Against this backdrop, the demand for healthy food continues to rise, leading to significant shifts in consumer purchasing behavior (Ding et al., 2022). However, numerous factors impact consumers’ decisions regarding healthy food consumption, resulting in a substantial disparity between consumption intentions and actual decisions (Ljubičić et al., 2023; Xu et al., 2023). Household consumption behaviors have been shown to impact resource consumption, environmental quality, and climate change. Changes in consumption behavior and willingness to purchase healthy foods can significantly contribute to sustainable development (Shahbaz et al., 2022). According to the precautionary saving theory, uncertainty in income and expenditure will increase residents’ precautionary savings and reduce residents’ current consumption. Improving the social security system can alleviate the uncertainty of income and expenditure, reduce precautionary savings, and increase residents’ consumption (Liu and Hu, 2022). Therefore, one of the solutions to the problem of stimulating healthy food consumption is reducing residents’ income and expenditure uncertainty by improving the social security system. Whether the social security system addresses the gap between intention and decision-making and promotes healthy food consumption at home still requires in-depth discussion and evaluation. In summary, formulating and implementing a scientific and adequate social security system to promote citizens to narrow the gap between consumption intentions and actual decision-making is a challenge facing the Chinese government.
Healthy food consumption encompasses individuals’ daily choices and purchases to provide nutrition, promote health, and prevent diseases. The primary objective of healthy food consumption is to fulfill the body’s requirements for a range of nutrients through a well-balanced and diverse diet (Kennedy et al., 2023; Le et al., 2023). Emphasizing the intake of various nutrients, including carbohydrates, proteins, fats, vitamins, and minerals, healthy food consumption aims to ensure the body’s normal functioning and overall wellbeing (Caso et al., 2022). It advocates the inclusion of a variety of foods such as fresh fruits, vegetables, whole grains, healthy protein sources (e.g., fish, chicken, beans), and moderate amounts of healthy fats (Sim and Cheon, 2019). Healthy food consumption also encourages the reduction of processed foods with excessive ingredients like high sugar, high salt, high fat, and artificial additives to mitigate the risks of obesity and other health issues associated with overconsumption (Werthmann et al., 2023).
Health is an essential factor affecting personal and family consumption. Developing the consumption habit of purchasing healthy food can improve the body’s immunity and reduce unnecessary medical expenses. On the contrary, health risks may squeeze consumer demand and disincentive affect consumer behavior. Long-term care insurance (LTCI) is vital in resisting economic losses or care burdens caused by risks such as poor health and disability. As a result, LTCI has increasingly become a focal point in discussions on social security, health consumption, and medical care in recent years (Ameriks et al., 2020). This insurance system, already implemented in countries such as Japan, South Korea, and the United States, is designed to offer financial support and services to elderly and disabled individuals—those with long-term care needs (Liu et al., 2023). Implementing LTCI can potentially lead to heightened awareness of health status and long-term care requirements, influencing people’s demand for and consumption of healthy food. In theory, LTCI has the potential to decrease unforeseen household expenditures, resulting in a reduction of precautionary savings in the current period and an increase in the net income and consumption level of elderly households (Imrohoroǧlu and Zhao, 2018; Liu et al., 2023). Beyond its direct impact on household finances, implementing LTCI will likely have a discernible effect on consumer behavior (Kopecky and Koreshkova, 2014).
Consumers are more concerned about health and long-term care-related products and services, tend to choose insurance products with comprehensive coverage, increase the demand for healthy food and medical care equipment, and increase their purchasing power due to financial support (Bronchetti, 2012; Lachowska and Myck, 2018; Liu et al., 2023). The introduction of LTCI policies has led to a deeper understanding of the importance of elderly care and disease management (Ameriks et al., 2020). Consumers are more aware that they may need LTCI and, therefore, are more inclined to choose products and services related to health and long-term care in their purchasing decisions (Feng Z. et al., 2020). Implementing LTCI policies has made people pay more attention to health issues and realize the importance of diet to health (Kim and Mitra, 2022). Therefore, by participating in LTCI policies, consumers may be more inclined to choose healthy food consumption in their purchasing decision-making behavior to maintain good health and prevent diseases. Based on the above logic, we use the ten-issue panel data of the China Health and Nutrition Survey (CHNS) from 1989 to 2015 and adopt a difference-in-difference (DID) framework to conduct an empirical analysis on the impact of healthy food consumption on households participating in the LTCI pilot and analyze the heterogeneous impact of consumption behavior.
This study is one of the few endeavors employing representative microdata from China to scrutinize the effects of LTCI policies. More significantly, it bears substantial policy implications for fostering healthy dietary choices. Based on the study findings, policymakers can provide appropriate recommendations for transforming public demand for medical care and promoting daily healthy food consumption, thus effectively enhancing individuals’ physical wellbeing. Balancing the promotion of a healthy diet with household consumption budget constraints is a universal challenge in health. As highlighted by Cutler (2010), scholars recognize the potential avoidance of malnutrition and unhealthy diet-related issues. However, consensus on effective avoidance strategies remains elusive. Our findings underscore that the nascent LTCI policy in China is an effective catalyst for reshaping consumer behavior, steering it toward healthier food consumption. This finding aligns with the current trajectory of China’s medical service delivery system reform, emphasizing resident health over mere service provision. Consequently, this study provides a valuable reference for ongoing policy formulation to enhance the dietary quality of families in China.
2 Literature review
2.1 Research on consumer behavior and healthy food consumption
Consumption behavior is the main driving force for consumption decisions, and consumers’ preferences for goods will affect actual consumption (Lee and Yun, 2015; Wang and Li, 2023). As people’s awareness of health increases, more and more consumers begin to pay attention to their eating habits and health status (Luo et al., 2021). Against this background, the demand for healthy food continues growing, and consumer purchasing behavior has undergone significant changes (Ding et al., 2022). Healthy food consumption has become an important trend in today’s society, representing people’s pursuit of health and longevity (Eyinade et al., 2021). Most studies show that consumers are increasingly inclined to choose healthy foods because they realize the importance of diet for good health (Eyinade et al., 2021; Ding et al., 2022; Ghufran et al., 2022). Consumers pay more attention to nutritional value and are more willing to pay more time and money for high—quality, healthy food (Ljubičić et al., 2023). Consumer purchasing behavior is often affected by many factors. First, personal health awareness and health knowledge play a crucial role in consumer purchasing behavior (Parashar et al., 2023). During the COVID-19 pandemic outbreak, people suffered economic turbulence, social instability, and food insecurity (Shahzad et al., 2021). A few studies have discussed the relationship and impact of COVID-19 on food insecurity, food purchasing costs, and online food purchase behavior. Adverse income shocks and unemployment have affected the cost of food purchases and made it difficult for people to afford healthy food, further causing malnutrition and personal health (Shahzad et al., 2023). With the hardship behind us, the emphasis on health and the demand for healthy food has increased. In addition, the quarantine of the epidemic drove online consumption, and consumers’ purchasing behavior shifted from offline to online. Shahzad et al. (2022) found that consumers purchasing healthy online food increased dramatically. The research of Yang et al. (2023) pointed out that consumers’ understanding of healthy foods has gradually increased with the popularization of health education and the dissemination of information. They pay more attention to the nutritional content and choose healthy foods that meet their needs through comparison and evaluation (Xu et al., 2023).
Secondly, advertising and publicity also influence consumer purchasing behavior (Boyland et al., 2016). Food manufacturers and sellers convey information about healthy food to consumers through various channels and methods. Advertisements emphasize products’ healthy ingredients, functions, and effects, establishing consumers’ health-related perceptions and expectations (Royo-Bordonada et al., 2016). These advertisements often influence consumers and regard them as essential references for purchasing decisions. In addition, the rise of social media has also had a massive impact on consumer purchasing behavior (Singh and Glińska-Neweś, 2022). People share their dietary preferences, healthy eating experiences, and purchasing experiences on social media, which provides opportunities for other consumers to refer to and learn from (Xu et al., 2023). Consumers can learn about other people’s reviews and recommendations of healthy foods through social media, influencing their purchasing decisions.
Finally, price and convenience are also important factors consumers consider when purchasing healthy foods (Bai et al., 2021). Although the development of the health food market has made such products more popular and diversified, their prices are often relatively high (Dominguez-Viera et al., 2022). Consumers need to make a trade-off between health and the economy and choose healthy foods that suit them. In addition, the convenience of purchasing healthy food is also an important factor for consumers to consider. In modern life with busy work, consumers are more inclined to choose healthy, convenient, and accessible foods (Goossensen et al., 2023).
2.2 Research on LTCI policy, consumer behavior and healthy food consumption
The above analysis shows that factors such as consumers’ health awareness, health knowledge, advertising, social media, price, and convenience jointly affect consumers’ decision-making on healthy food consumption. The emergence of the LTCI policy provides families with financial support and services (Imrohoroǧlu and Zhao, 2018; Liu et al., 2023). Existing research focuses on the following aspects. First, LTCI policies can increase people’s attention and awareness of health. Liu et al. (2023) believe that since long-term care insurance targets groups prone to disease, such as the elderly, these groups pay more attention to their health conditions and long-term care needs. They are usually more inclined to choose healthy foods to maintain good health and reduce disease risk. Secondly, the LTCI policy has spawned a huge long-term care service market, including health food and related industries (Fu et al., 2017). As the need for LTCI, so does the demand for care services and products (Lei et al., 2022). This provides enormous business opportunities for healthy food production and sales companies. Third, LTCI policy emphasizes prevention and health management (Feng J. et al., 2020). The policy encourages people to adopt a healthy lifestyle, including a reasonable diet and balanced nutrition. Under the guidance of policies, people have paid more attention to dietary health and begun to pay more attention to food selection and consumption (Zhu and Österle, 2017). They are more inclined to buy healthy foods, such as organic foods, natural foods, low salt and low sugar foods, etc., to maintain good health and reduce disease risk. Finally, the LTCI policy promotes increased healthy food consumption through economic support (Liu et al., 2023). LTCI provides financial subsidies and services to eligible beneficiaries, allowing them to pay for long-term care-related expenses better (Kim and Mitra, 2022), which also means they have more financial ability to purchase healthy foods and improve their diet.
3 Background
3.1 LTCI policy background
LTCI usually refers to a social insurance system that raises funds through social mutual aid to provide funds or service guarantees for the primary life care of middle-aged and elderly disabled people and medical care closely related to bear life (Liu et al., 2023). Many countries, including Germany, Japan, and the Netherlands, have established different long-term care insurance systems internationally. Qingdao, China, learned from other countries’ LTCI implementation experience and issued the “Opinions on Establishing a Long-term Medical Care Insurance System (Trial)” in 2012, leading in implementing the LTCI system in cities and towns. In 2015, this system was expanded to rural areas, becoming the first region in the country to achieve full coverage of LTCI. In 2016, China issued the “Guiding Opinions on Carrying out the Pilot Program of Long-term Care Insurance System,” and 15 cities began to pilot the LTCI system. In September 2020, the National Medical Security Administration issued the “Guiding Opinions on Expanding the Pilot Program of the Long-term Care Insurance System”, adding 14 pilot cities. In 2022, the State Council of China issued the “14th Five-Year Plan for National Aging Development and Elderly Care Service System”, proposing to steadily establish the LTCI system and improve the LTCI handling service system. In 2022, the China Banking and Insurance Regulatory Commission issued the “Notice on Carrying out the Pilot Program of Liability Conversion Business between Life Insurance and Long-term Care Insurance” to guide life insurance companies to carry out the pilot program of liability conversion business between life insurance and LTCI and increase the supply path of commercial LTCI. Twelve years have passed since the first batch of pilot policies were introduced, and China’s LTCI protection results are beginning to show. According to data from the “2021 National Aging Development Bulletin”, as of the end of 2021, a total of 144.607 million people in China have participated in LTCI, enjoying The number of people receiving benefits was 1.087 million, the fund income for the year was 26.06 billion yuan, and the fund expenditure was 16.84 billion yuan.
Currently, China’s LTCI has the following characteristics: First, the funding source of LTCI in various pilot areas is mainly from the medical insurance coordination fund, supplemented by unit supplementary medical insurance, individual new contributions, and financial subsidies. Fund disbursements are closely tied to disability assessments and payment criteria (Luo et al., 2024). Second, the scope and degree of protection continue to deepen (Lei et al., 2022). The scope of protection in pilot cities such as Guangzhou and Shangrao has been expanded from those insured by the basic medical insurance for urban employees to those insured by the basic medical insurance for urban and rural residents. Based on protecting the severely disabled groups, pilot cities such as Chengdu and Qingdao have gradually included groups with moderate to mild disabilities and dementia. Third, the security model mainly includes institutional care and home care. Some pilot cities are further refined. For example, Jingmen in Hubei is divided into four categories: home-based part-time, home-based full-time, elderly care institutions, and medical institutions, and Beijing Shijingshan is divided into three categories: home-based self-care, home-based care, and institutional care.
3.2 Other existing food consumption policies
Since 2001, the Chinese government has promulgated the “Regulations on the Safety Management of Genetically Modified Organisms”, the “Measures for the Safety Management of Agricultural Genetically Modified Organisms,” the “Measures for the Safety Management of the Import of Agricultural Genetically Modified Organisms,” and the “Measures for the Management of the Labeling of Agricultural Genetically Modified Organisms.” The above regulations and “Measures” implement different management methods for importing, exporting, and transiting genetically modified agricultural products. Among them, the focus of control is importing genetically modified agricultural products. The control measures are implementing a safety-graded management evaluation system and a mandatory labeling system for imported products (Sun et al., 2021). On the one hand, the supply of raw materials in the feed industry and soybean crushing industry continues to increase, which promotes the rapid development of domestic livestock, livestock, and poultry breeding industries and ensures sufficient domestic supply of meat, eggs, oils, and milk. On the other hand, the large-scale import of genetically modified products has lowered the price of genetically modified products and reduced the input costs of domestic livestock, animal husbandry, and poultry breeding industries. Due to the stickiness of food prices in the short term, competitors will produce more related products, decreasing related food prices and reducing the marginal budget share of related food for urban residents. Implementing the mandatory labeling system for genetically modified foods has both a positive promoting effect and a negative inhibiting effect on the marginal budget share of urban residents’ relevant food.
In terms of green food consumption, China has successively promulgated several green food policies in recent years, such as the “2021 Action Plan for Standardizing the Use of Green Food Labels” and the “Outline of the 14th Five-Year Plan Development Plan for the Green Food Industry”. These policies are mainly supply-side policies that use market supervision to affect producer investment, production costs, and access conditions, and demand-side policies such as publicity and promoting consumer consumption tendencies and behaviors. They are binding policies that set standards and regulate certification (Zhu et al., 2013). These policies focus on food safety and quality, vigorously promote the development of the green food market, effectively improve consumers’ environmental awareness and information acquisition capabilities, and improve the current situation where consumers do not understand and do not trust green food.
4 Methodology
4.1 Data source
This study used panel data from the ten issues of the China Health and Nutrition Survey (CHNS) from 1989 to 2015. CHNS is a long-term, national-level population health survey project commissioned by the University of North Carolina in the United States and the Ministry of Health of China. The project began in 1989 to understand the Chinese population’s nutritional status, health status, and lifestyle and the impact of these factors on chronic diseases. The project has spanned over 30 years and has become one of the world’s most influential population health survey projects. CHNS uses a multi-stage sampling method to select representative samples from various cities and villages in China and collects data on individuals, families, and communities through face-to-face questionnaires and biometric measurements. The survey contains basic personal information, such as diet, nutrition, lifestyle, health status, medical care, and other aspects. CHNS adopts the principle of multi-stage sampling method. In terms of cities, provincial capital cities were selected, and one medium-sized city with poor economic development was randomly selected. In rural areas, counties in the province are divided into three categories: high, medium, and low levels of economic development. One county is selected from each high-level and low-level category, and two counties are selected from the medium-level categories. Four survey points were determined in each city or county based on a random multi-stage cluster sampling. The city selected two urban neighborhood committees and two suburban villages, and the county selected one neighborhood committee and three villages where the county government is located. The survey is divided into three scales: community, household, and individual. CHNS considers macro factors such as China’s geographical environment, economic development level, population distribution characteristics, and urban and rural structure differences, covering China’s eastern, central, western, and northeastern regions. This data highly represents China’s overall situation and is highly authoritative and reliable (Chen et al., 2023). The content of CHNS involves nine major parts, including nutritional diet, health care and medical insurance, daily activities, and physical condition. The data in this article mainly applies to the nutritional dietary structure survey part of CHNS. The nutritional dietary structure survey uses a continuous 3-day, 24-h recall method to collect food intake information of family members aged two and above in all surveyed households. The main survey indicators include household food consumption in 3 days, statistics per person per day, name of daily meals, preparation method, preparation place, eating time, etc. This data can be used to measure the consumption of healthy food among urban and rural residents in China. Therefore, the CHNS database is a good fit for the topic of this study.
Moreover, the LTCI policy in this study was piloted in 2012, and the time node of the CHNS data meets the research requirements, providing a double difference setting for this article. The reason is that the CHNS data’s time node is consistent with this policy’s implementation time. This temporal coincidence provides us with a setting for DID analysis. DID can evaluate the impact of the LTCI policy on research subjects by comparing the differences before and after the implementation of the policy and between the treatment group and the control group affected by the policy. Therefore, the consistency of the time nodes of the CHNS data with the pilot time of the LTCI policy can provide an effective research design, allowing us to use the DID method to evaluate the impact of the policy on the research objects. We eliminated data with missing values in household identification codes, food intake, preparation methods, and eating time, eliminated outlier samples with higher calorie intake than five standard deviations, and obtained 41,878 samples.
4.2 Identification strategy
The LTCI policy lasted for ten years in China, and there were significant regional differences. It was a standard quasi-natural experiment. The reasons why LTCI policy can be regarded as a quasi-natural experiment are: First, LTCI policy pilots are usually implemented by the government in specific regions or groups, and this selection is often based on specific standards or needs rather than random selection. Therefore, implementing this policy has a certain “naturalness” and is not entirely controlled by researchers (Lei et al., 2022). Second, when the LTCI policy is implemented on a pilot basis, there are usually other regions or groups where the policy has not been implemented, and these regions or groups can serve as control groups. Researchers can compare the differences between pilot areas and control groups before and after policy implementation to evaluate the effectiveness of the policy. Third, implementing LTCI policy pilots allows researchers to compare changes before and after implementation in the same region or population. Such time series comparisons help identify the impact of policies. Finally, because LTCI policy pilots are conducted under real-world conditions, the results tend to have high external validity, that is, the research findings can be better generalized to other similar situations. The above four characteristics of LTCI policy are consistent with the definition of the quasi-natural experiment.
This study divided the sample into households affected by LTCI policy (experimental group) and households unaffected by LTCI policy (control group). The DID method was used to identify whether implementing LTCI affected household healthy food consumption. DID is an econometric method used to evaluate the effectiveness of policies or interventions. This method estimates the causal effect of a policy by comparing changes before and after the policy is implemented (differences in time) and changes between a group that implements the policy and a control group that does not implement the policy (differences between groups) (Bertrand et al., 2004; Ma et al., 2023b). The principle of DID is to calculate the changes in the experimental group before and after the policy is implemented (the first difference), then calculate the changes in the control group during the same period (the second difference), and finally calculate the difference between the two differences (i.e., the experimental group’s change minus the change in the control group). This result represents the net effect of policy implementation, that is, the effect after removing the effects of time trends and other non-policy factors. DID is suitable for this study because LTCI policy pilots are often conducted in specific regions, which provides conditions for selecting experimental and control groups, making DID a suitable tool for evaluating policy effects. We refer to the method of Liu et al. (2023) and set the baseline regression as follow Equation (1):
Yit=a0+βLTCIi×Postt+γXit+ηi+ωt+εit (1)
where, Yit represents healthy meal preparation methods, whether the meals are processed foods, daily meal quantity, and the number of healthy preparation methods in the daily meal quantity. These indicators indicate household consumption of healthy foods. LTCIi×Postt is the interaction term of the dummy variable before and after the treatment group implements the LTCI policy. The interaction term coefficient β is this study’s core coefficient of concern, representing the difference in outcome variables between households and other regions caused by participation in the LTCI policy. Based on this, we examine the policy effect of LTCI, that is, whether LTCI affects household consumption behavior and healthy food consumption. Xit is a set of control variables at the family level, including gender, place of birth, marital and ethnicity, family income and work intensity, self-rated health, disease history, tobacco and alcohol history, household cleaning water, and household hygiene. By controlling the above variables, this study can more accurately estimate the impact of implementing LTCI on household consumption behavior and healthy food consumption while reducing the bias caused by these unobserved confounding variables (Chen et al., 2023). In this way, the findings are more likely to reflect the effects of long-term care insurance policies themselves rather than the effects of other related factors. The specific reasons and measurement methods for selecting these variables are detailed below. ηi is the individual fixed effect. ωt is the year-fixed effect. εit represents the disturbance term and uses robust standard errors clustered on the household dimension to alleviate the impact of individual-level related factors on the estimation results.
4.3 Variable selection and processing
4.3.1 Dependent variable (Yit)
This study refers to the research ideas of previous literature (Feng J. et al., 2020; Dominguez-Viera et al., 2022; Le et al., 2023; Werthmann et al., 2023). Meal preparation methods (HMPM) are dummy variables indicating that households used healthy cooking methods to prepare their daily meals in the year of the survey. CHNS data includes cooking methods such as boiling, stir-frying, frying, steaming, drying, cooked food, baking, and raw eating. Healthy food preparation methods include boiling, steaming, and raw eating. This study states that when family meals are prepared using these three methods, the value of Healthy meal preparation methods is 1; otherwise, it is 0. Whether the meal is processed food (NPF) is a dummy variable indicating whether the family often consumes processed food in their daily meals in the year of the survey. This study sets the value of Non-processed food as 1 when the family diet does not include processed food; otherwise, it is 0. Daily meal quantity (DMQ) is a household’s total daily meal intake in the year of the survey. CHNS data reports households’ total daily food consumption in grams. This study uses the natural logarithm to measure daily meal quantities. The reasons for using natural logarithm to measure are: First, this method can reduce the impact of large differences in actual values in CHNS data on regression, making the data distribution closer to a normal distribution. Second, after log transformation, the coefficients of the model estimates can be interpreted as percentage changes, which is a common way of interpretation in economics. Third, logarithmic transformation can linearize nonlinear relationships, allowing linear models to fit the data better. In economic and social science research, many relationships between variables may be nonlinear on the original scale, and log-transformed linear relationships are more accessible to interpret and model. The number of healthy food preparation methods in the number of daily meals (HFC) is the interaction term between the number of meals a household consumes daily in the year of the survey and whether it is processed food. It is used to reflect the structure of healthy food consumption. The reasons for using interaction terms to measure are: first, healthy food consumption depends not only on the quantity of food but also on the quality of the food. Processed foods are often considered less healthy than fresh foods. For example, when the number of meals per day increases and the number of processed foods decreases, the interaction term between them reflects a healthier food consumption structure in the household. Therefore, the interaction term can help us accurately measure households’ healthy food consumption structure. Second, interaction terms can reveal household behavioral patterns when consuming different types of food. For example, households may have different consumption tendencies when consuming processed and non-processed foods, and this difference can be captured through interaction terms. Third, if implementing LTCI causes households to be more inclined to consume healthy foods, this change may manifest in households reducing their consumption of processed foods while increasing their consumption of non-processed foods. The interaction term can serve as an indicator of this behavioral change. Fourth, without interaction terms, meal size or processed food variables alone may not adequately control other factors influencing healthy food consumption. Interaction terms can control these potential confounders and provide more accurate estimates.
4.3.2 Independent variable (LTCIi×Postt)
LTCIi is a dummy variable indicating whether the household belongs to the four provinces and cities of Beijing, Jiangsu, Shandong, Shanghai, and Chongqing. Postt is a dummy variable for policy implementation. Since there are differences in policy implementation time among provinces and cities, this study assigns values based on the actual implementation time. Specifically, when t≥2012, the Postt value corresponding to Beijing is 1; when t≥2013, the Postt value corresponding to Jiangsu and Shandong is 1; when t≥2014, the Postt value corresponding to Jiangsu and Shandong is 1; when t = 2015, the Postt value corresponding to Chongqing is 1; otherwise, the value of postt is 0.
4.3.3 Control variables
We drew on relevant studies (Zhu and Österle, 2017; Min et al., 2021; Chen et al., 2023; Fang et al., 2023) and selected the following control variables at the household level. There may be differences in the consumer behavior of men and women, including preferences for healthy foods and purchasing decisions. Therefore, the gender of the household head (Gender) is measured according to the CHNS statistical indicators: male is 1 and female is 2. Different regions may have different eating habits and types of food available, which may affect household food consumption. Therefore, the birthplace (Birthplace) of the household head is measured according to the CHNS statistical indicators, that is, if he was born in a town, it is 1, otherwise it is 0. Married or partnered individuals may have different consumption patterns, particularly food purchases and household expenditures. Therefore, the household head’s marital status (Marry) is measured as 1 according to the married value set in CHNS and 0 otherwise. Families of different ethnic backgrounds may have different eating habits and cultural preferences, affecting their food choices. Therefore, the ethnic group (Ethnic) of the household head is measured as 1 according to the ethnic minority set in CHNS and 0 otherwise. Income level is an essential factor affecting spending power and consumption choices, and high-income families may be more inclined to purchase healthy foods. Therefore, the family’s annual income (Income) is measured by summing up the various household income statistics from CHNS and taking the natural logarithm. Individuals with high work intensity may have less time to prepare healthy foods, affecting healthy food consumption at home. Therefore, the family work intensity (Activity Level) is measured according to the CHNS statistical indicators, that is, the value of moderate physical activity and below and the inability to work is 1; otherwise, it is 0. Individuals’ health evaluations may influence their lifestyle and food consumption choices. Therefore, the self-evaluation of family health (Self-health evaluation) is based on the indicators of CHNS statistics (compared with other people of the same age, how do you think your current health status is?) and the choice of “very good” and “good” is 1, otherwise 0. Family members with a history of illness may require special diets, which can affect the family’s food consumption patterns. Therefore, the family’s medical history is measured according to the CHNS statistical indicators, that is, the value of family members suffering from chronic diseases, hypertension, diabetes, myocardial infarction, stroke, tumors and other diseases is 1, otherwise it is 0. Smoking and drinking habits may be associated with unhealthy lifestyles, which may affect household demand for healthy foods. Therefore, the family’s tobacco and alcohol history (Tobacco and alcohol) is measured according to the CHNS statistical indicators, that is, the value of a family member who smokes and drinks more than 2 times a month is 1, otherwise it is 0. Household cleaning water and sanitation conditions may affect family members’ health status and demand for healthy foods. Therefore, whether a household uses clean water (Cleaning water) is measured according to the CHNS statistical indicators (the value of using clean tap water is 1. Otherwise, it is 0). Home hygiene is measured according to the CHNS statistical indicators, that is, if there is little or no feces around the room, the value is 1, otherwise it is 0. Descriptive statistics of the above variables are shown in Table 1.
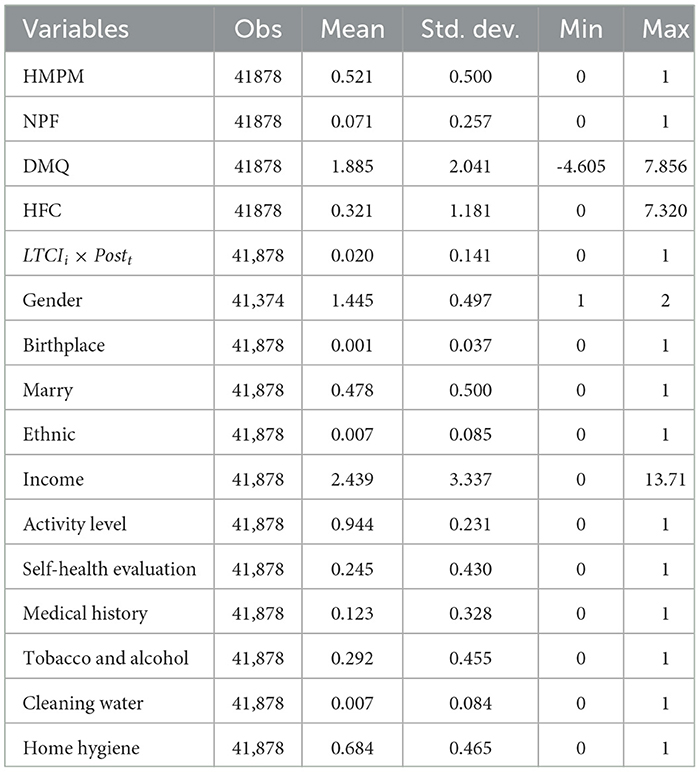
Table 1. Descriptive statistics.
4.4 Variable mean test
This study uses the mean test to determine whether there is a significant difference in the overall means represented by the experimental and control groups. Table 2 reports the statistical characteristics of the differences between the control and experimental groups. Among them, the healthy food consumption of households participating in the LTCI policy is greater than that of non-participating households. This result shows the difference in changes in healthy food consumption between Chinese households before and after receiving treatment and households that did not participate in other cities. However, the impact LTCI has had remains to be seen. Further empirical analysis is needed later. There are no significant differences in gender and tobacco and alcohol history of household heads participating in the LTCI policy, indicating that these two characteristics will not change due to policy implementation. Most variables have increased significantly compared with before participating in the LTCI policy. Therefore, the control variables selected in this study can effectively control the inherent differences between the control and experimental groups, thereby obtaining more reliable policy effect evaluation results.
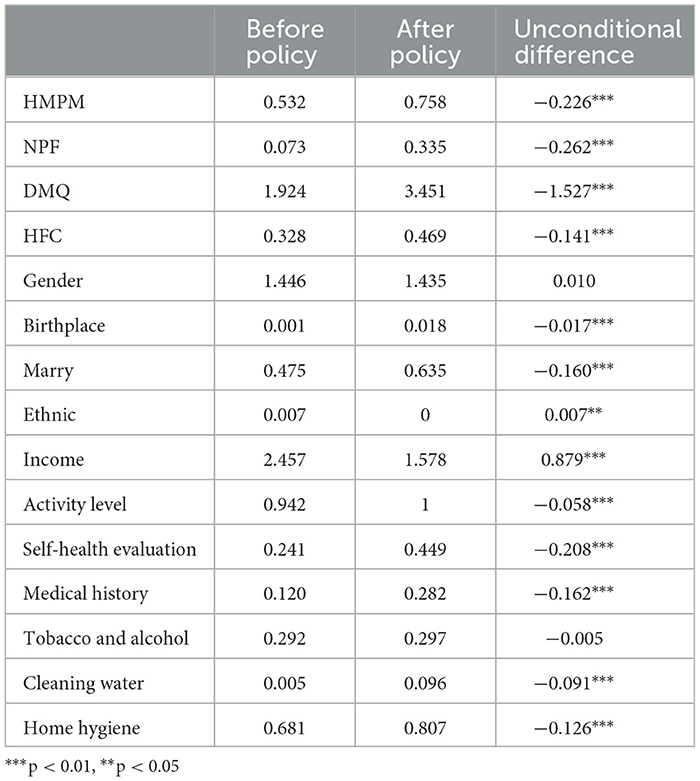
Table 2. Variable group mean test.
5 Results
5.1 The impact of LTCI policy on healthy food consumption among Chinese households
According to the empirical method introduced above, this article uses Stata17 software to comprehensively identify whether implementing the LTCI policy affects household healthy food consumption. The empirical results are shown in Table 3.
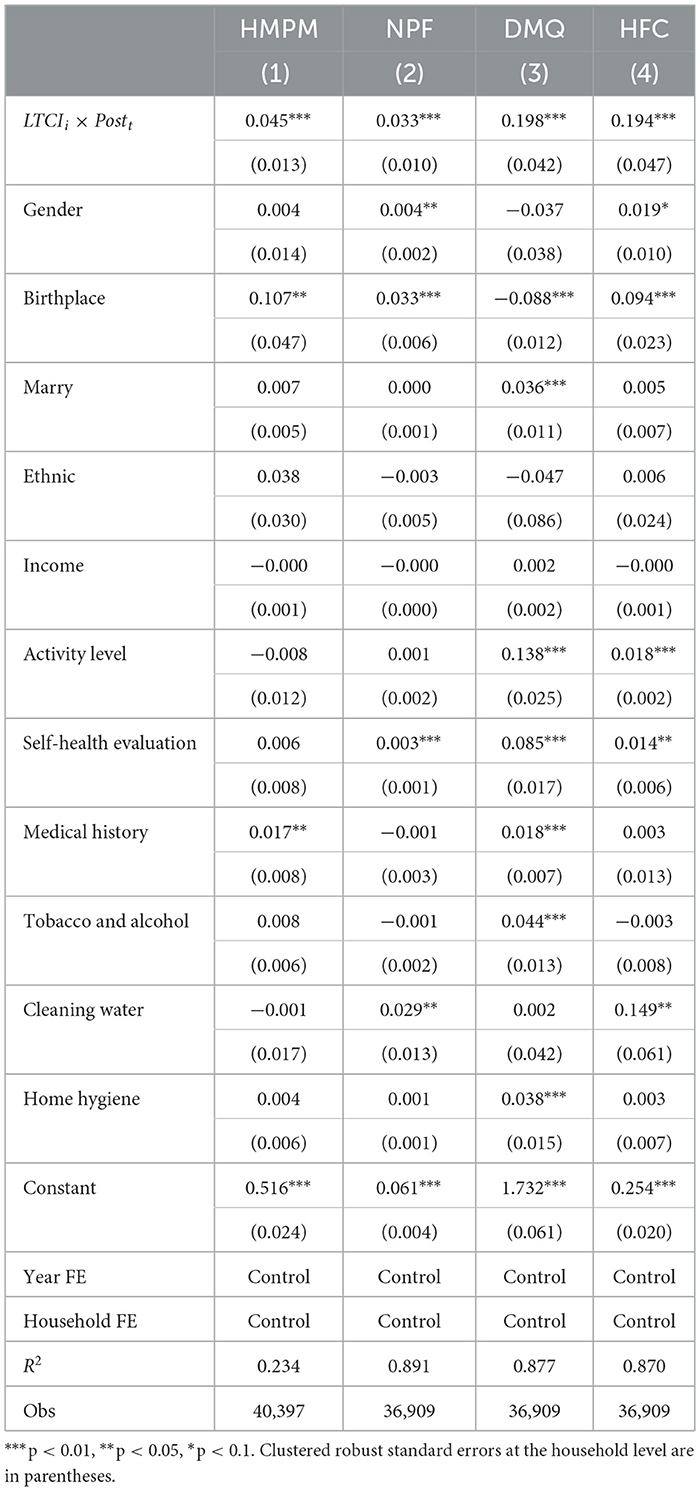
Table 3. Difference-in-differences regression results.
It can be found from column (1) of Table 3 that the estimated coefficient of LTCIi×Postt is significant at 0.045 at the 1% significance level. This result shows that implementing LTCI can increase the frequency of adopting healthy diet preparation methods by 0.045 times for families participating in the policy compared with families not participating. This result means that implementing LTCI policies may prompt families to adopt healthier diet preparation methods, thus positively impacting families’ eating habits and health. Column (2) shows that the estimated coefficient of LTCIi×Postt is significant at 0.033 at the 1% significance level. This result shows that implementing LTCI can increase the frequency of diets that do not include processed foods for households participating in the policy by 0.033 units compared with households not participating. Considering that processed foods often contain more additives and high-calorie ingredients, this change may help families eat healthier and reduce the negative health effects of processed foods. Column (3) shows that the estimated coefficient of LTCI is significant at 0.198 at the 1% significance level, indicating that implementing LTCI can increase the daily meal consumption of households participating in the policy by 0.198% compared with households not participating in the policy. After conversion into actual dietary consumption, households participating in the policy increased their daily dietary consumption by an average of 1.219 grams compared with households not participating in LTCI. This result means that LTCI policies may prompt households to increase their food consumption by a certain amount in their daily meals. In a practical sense, this may mean that households purchase more fresh ingredients or higher-quality food when financial conditions allow, thereby improving their diet and nutritional intake. Column (4) still shows that the estimated coefficient of LTCIi×Postt is significant at 0.194 at the 1% significance level. This result shows that overall, implementing LTCI can increase the healthy food consumption structure of households participating in the policy by 0.194 units compared with households not participating. The practical implication of this result is that LTCI policies may impact households’ dietary patterns, especially regarding processed foods. Households participating in the policy are more likely to consume less processed food or to pay more attention to quantity and quality when consuming processed food. Considering the potential health effects of processed foods, this change may help families improve their diets, reduce the adverse health effects of processed foods, and improve overall nutritional status. The regression results show that participating in LTCI policies can effectively increase Chinese families’ healthy food consumption. Next, we analyze how LTCI participation may influence healthy food consumption behavior.
5.2 Mechanism test
The above simple analysis shows that risk prevention is the primary purpose of LTCI, and implementing LTCI can increase the consumption of healthy food related to future disability risk. In order to verify this mechanism, this paper conducts regression using self-rated health as the mediating variable. The mediating effect model is usually used to study how one variable affects another mediating variable, thereby affecting the outcome variable (Yang and Ma, 2023). We construct the following mediating effect model [Equation (2) and Equation (3)]:
Mit=a1+ϕ1LTCIi×Postt+γXit+ηi+ωt+εit (2)
Yit=a2+ϕ2LTCIi×Postt+δMit+γXit+ηi+ωt+εit (3)
where, Mit is the mediating variable, that is, the family’s self-evaluation of health (Self-health evaluation). Suppose ϕ1 passes the significance test. In that case, a relationship exists between implementing LTCI and the family’s self-rated health, and the mediation effect is initially established. Then, if ϕ2 and δ both pass the significance test, the mediation effect mechanism is established. LTCI affects the family’s healthy food consumption by affecting the family’s self-evaluated health. The regression results are shown in Table 4.
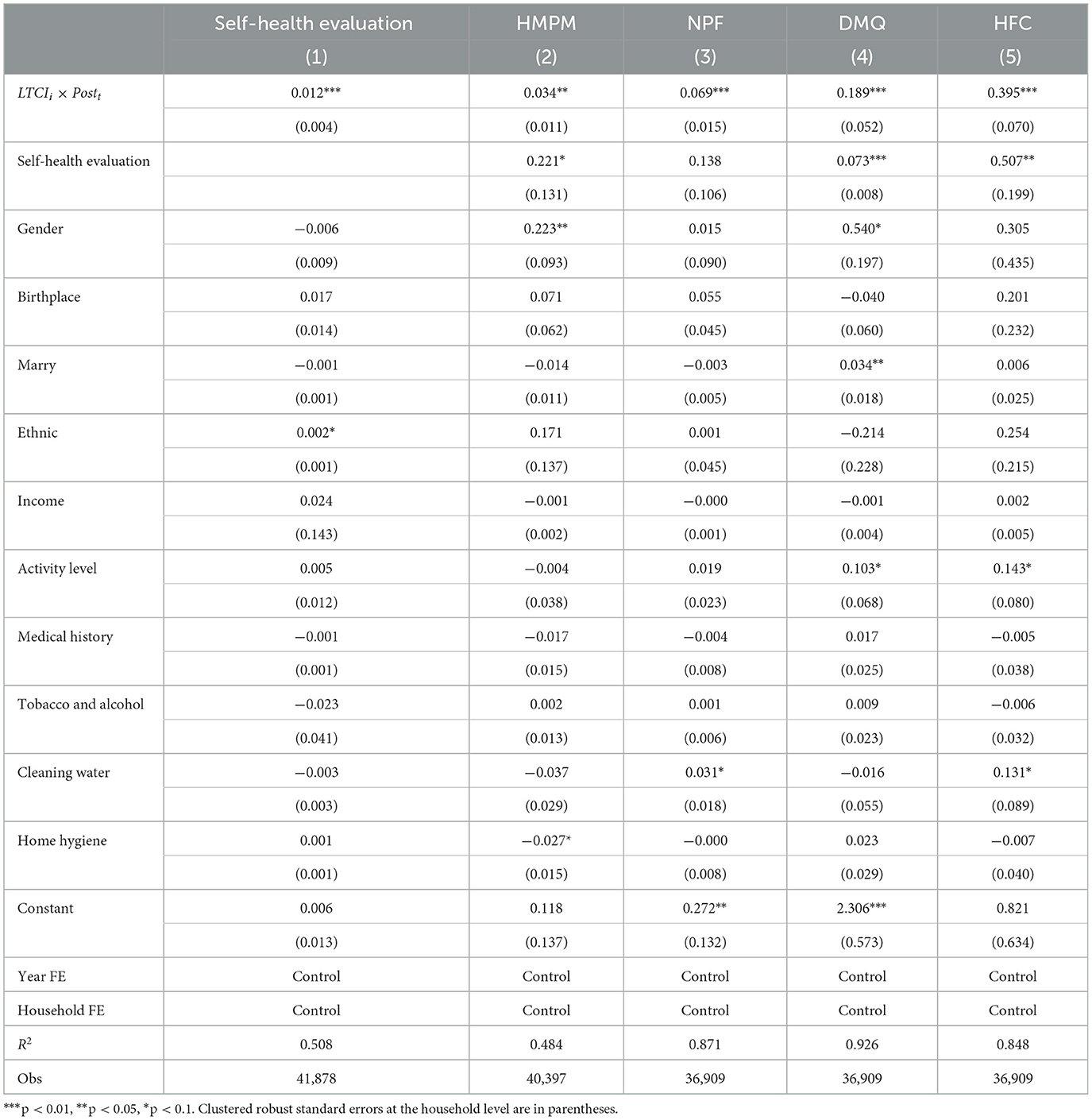
Table 4. Mechanism test.
Column (1) shows that the estimated coefficient of LTCI is significantly 0.012 at the 1% significance level, indicating that LTCI effectively improves the self-rated health of families, consistent with existing research findings (Imrohoroǧlu and Zhao, 2018). Except for column (2), which does not pass the mediating effect test, the others all pass the mediating effect test. It is verified that LTCI increases families’ healthy diet preparation methods, daily meal consumption, and healthy food consumption structure through risk prevention mechanisms. Families often purchase LTCI to deal with underlying health problems and long-term care needs. Such insurance policies may remind families to pay more attention to health issues and enhance their health awareness, affecting household consumer behavior (Imrohoroǧlu and Zhao, 2018; Ariaans et al., 2021). Family members may be more inclined to choose healthy foods to maintain good health. In addition, by participating in LTCI, families may pay more attention to the importance of disease prevention and form healthy consumption behaviors (Liu et al., 2023). Healthy foods are often packed with nutrients that help boost immunity and reduce disease risk. As a result, households may increase their consumption of healthy foods to prevent potential health problems. Most importantly, participating in LTCI may require certain financial investments (Dominguez-Viera et al., 2022). In order to cope with potential medical and long-term care costs, households may re-evaluate their budgets, adjust consumption preferences and behaviors (Eyinade et al., 2021), and regard healthy food consumption as an essential expenditure item, resulting in households increasing their consumption of healthy foods. These results verify and supplement the existing literature on the effects of social insurance consumption channels.
5.3 Robustness tests
5.3.1 Parallel trend test
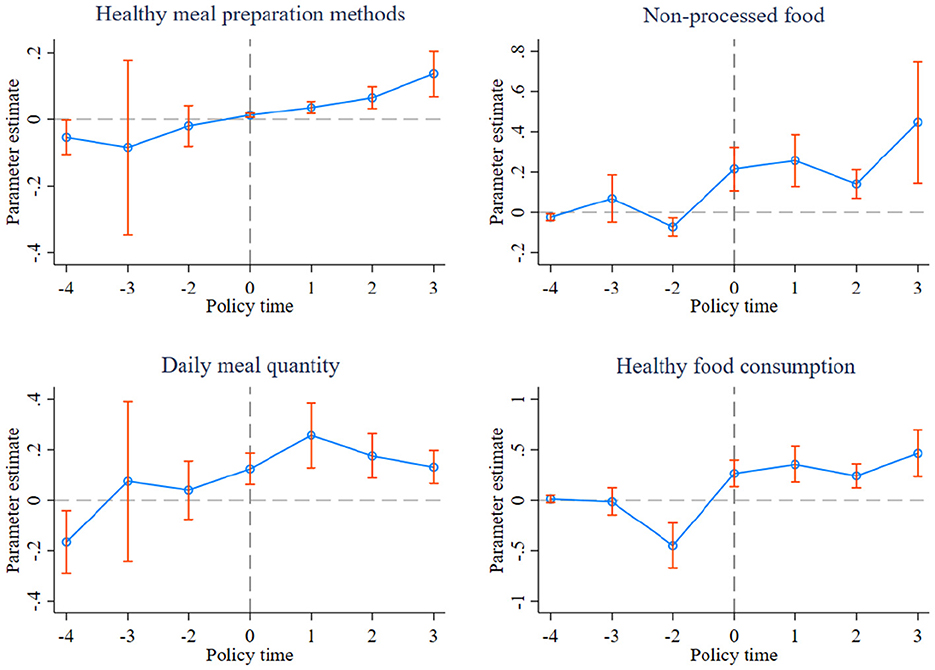
Parallel trend testing is an essential prerequisite for using the DID model. The primary purpose is to evaluate whether the impact of a particular policy, intervention, or event on a specific outcome variable is statistically significant (Ma et al., 2023b). In a parallel trend test, a control group and an experimental group are usually selected, and the trend of a certain outcome variable is used as the evaluation index. By comparing whether the trends of the treated group and the untreated group before a certain time point are parallel and whether the trend after that time point is significantly different, the size and statistical significance of the causal effect between the treatment group and the non-treatment group can be assessed. Parallel trend testing aims to reduce the confounding effects caused by other potential influencing factors to more accurately assess the impact of policies, interventions, or events on a specific outcome variable. This study conducted a parallel trend test by setting the base period to the year before LTCI was implemented.
Figure 1 reports the results of the parallel trend test. The changing trend of the estimated coefficients of LTCI on the four dependent variables in the three periods before the policy was implemented was relatively flat. It did not pass the significance test at the 1% level, indicating that before implementing the LTCI policy, the healthy food consumption of households in the control and experimental groups was not the same. There is no noticeable difference, satisfying the parallel trend assumption. In the year of LTCI implementation and subsequent years, household healthy food consumption in the experimental group increased significantly.
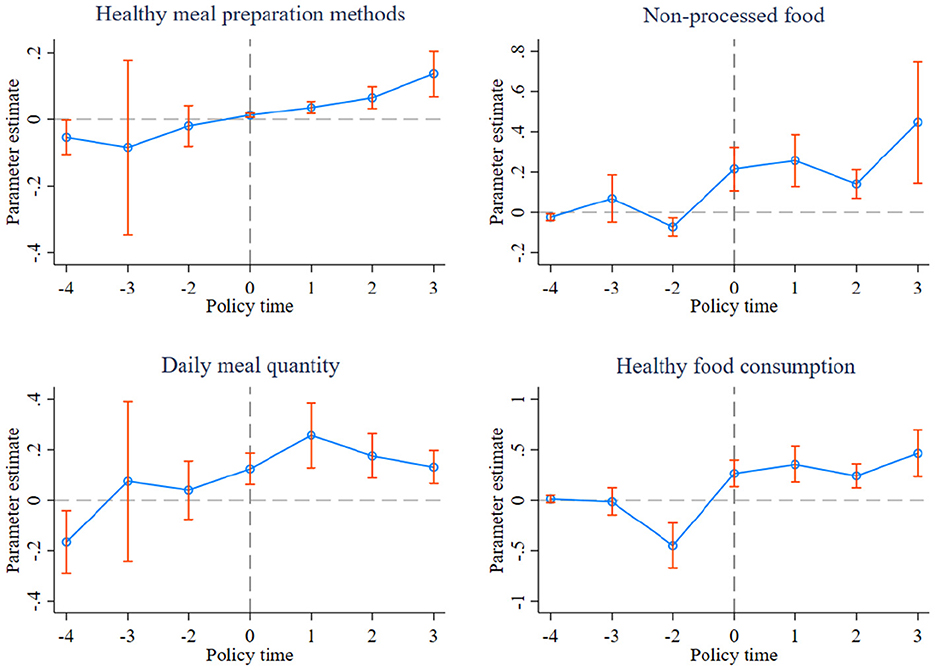
Figure 1. Parallel trend test.
5.3.2 Placebo test
Although this study has controlled a large number of household characteristic variables in a quasi-natural experiment, there may still be some non-observed household characteristic factors that affect the evaluation results of the LTCI pilot policy. A potential threat is that central and local governments may have selected pilot cities based on predetermined city-level characteristics and been assigned non-randomly. We address this issue with a placebo test. If the model is a simultaneous point DID, refer to Liu and Lu (2015) and randomly select provinces and cities equal to the number of real pilots from all samples as the experimental group. However, due to the differences in pilot policy impact time in multi-time point DID, it is necessary to randomly generate the pseudo experimental group dummy variable LTCIfalse and the pseudo policy impact dummy variable Postfalse at the same time, that is, randomly select a sample period for each sample object as its policy time. Based on this, we use the following placebo test method to further ensure the estimation results’ robustness. First, Stata software is used to construct 500 random shocks of the pseudo-LTCI pilot policy. Secondly, 1,700 households are randomly selected as the experimental group each time, and the policy time is randomly given, resulting in 500 groups of dummy variables LTCIfalse×Postfalse. Third, the kernel density of 500 LTCIfalse×Postfalse and its P-Value distribution are presented in the figure. The results are shown in Figure 2. The false estimated coefficients generated during random processing are concentrated near 0, and the P-value are mostly higher than 0. The estimated coefficient of the actual policy is significantly different from the placebo test results. This result also shows, to a certain extent, that the quantitative evaluation results of this article are not significantly affected by this potential factor. The results are robust.

Figure 2. Placebo test.
5.3.3 Semiparametric DID method
Similarly, this paper also conducts robustness testing through the semiparametric DID method (SDID) proposed by Abadie (2005). In the case of two periods of balanced panel data, this method uses weighting to balance the characteristics of the experimental and control group samples. It can be concluded that this method has a certain credibility even when the common trend is not completely satisfied. SDID is as follow Equation (4):
E[ΔYtP(dt=1)×dt−ψ(Xb)1−ψ(Xb)] (4)
where, dt represents whether it is the experimental group in period t, P(dt = 1) represents the probability of the experimental group, ψ(Xb) is the Abadie weight, which can be calculated through the linear probability model ψ(Xb) = P(dt = 1|Xb). Houngbedji (2016) believes that SDID is reliable because common trends cannot be guaranteed. Therefore, this article will use Abadie SDID for further verification. The results are shown in Table 5. On indicators such as Healthy meal preparation methods, Non-processed food, Daily meal quantity, and Healthy food consumption, the coefficients before DID of the interaction term are all significantly positive, and the results are consistent with the previous article.
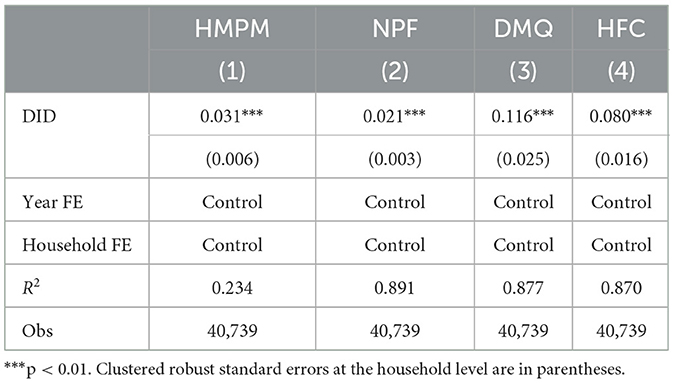
Table 5. Abadie SDID regression results.
5.3.4 Competitive policy: exclusion of free medical examination program
Since 2009, China’s national and local governments have successfully launched pilot policies on free physical examination programs. This policy aims to promote free physical examination services. The program covers urban and rural residents and provides comprehensive health check-ups, routine examinations, and joint disease screenings. The examination information is filled in the health examination form and included in the unified management of individual health files. Then, the examination doctor must promptly inform the community of the evaluation results and provide free corresponding health guidance and management. The implementation of the free physical examination program coincides with the implementation of the LTCI pilot policy, so it is necessary to isolate the impact of the free physical examination program on household consumption behavior. We added the year of implementation of the free physical examination program policy and the pilot area (FMEP) interaction term in the model to control its impact on the main estimated results. It can be found from the estimation results that after controlling for the free physical examination program (see Table 6), the estimated coefficients of LTCIi×Postt are still significantly positive, which shows, to a certain extent, that the LTCI policy has a noticeable effect on increasing healthy food consumption.
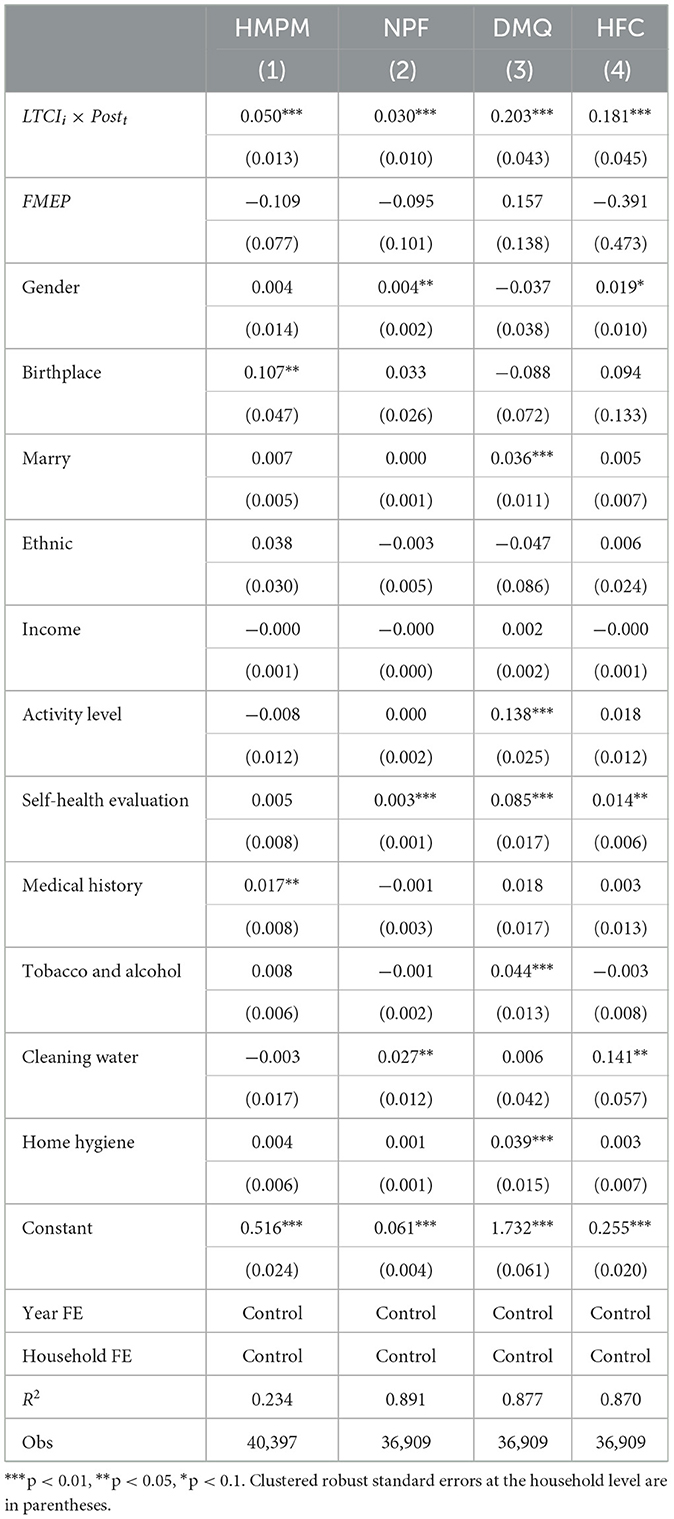
Table 6. A test of competitive policy: excluding the impact of free medical examination programs.
5.3.5 Competitive policy: exclusion of pharmaceutical price negotiations
Sichuan, Shandong, and Jiangsu implemented pilot drug price negotiations in 2010, 2012, and 2013, respectively. Pharmaceutical price negotiations may indirectly affect healthy food consumption, especially regarding chronic disease treatment. The policy aims to bring drug prices down and reduce the financial burden on individuals when purchasing drugs, thus freeing up more disposable income. This increases people’s spending on healthy foods as they can now spend more on healthier foods. Furthermore, success in pharmaceutical price negotiations may draw public attention to the healthcare system and drug pricing. This may increase people’s awareness of health issues and prompt them to pay more attention to their health. In this case, people may buy more healthy foods to improve eating habits, enhance immunity, etc. The implementation of pharmaceutical price negotiations happens to be during the implementation period of the LTCI pilot policy, so it is necessary to isolate the impact of pharmaceutical price negotiations on household consumption behavior. We added the year of implementation of the pharmaceutical price negotiation policy and the interaction term of the pilot area (PPN) in the model to control its impact on the main estimation results. It can be found from the estimation results that after controlling for pharmaceutical price negotiations (see Table 7), the estimated coefficients of LTCIi×Postt are still significantly positive, indicating LTCI policy still has a robust effect on increasing healthy food consumption.
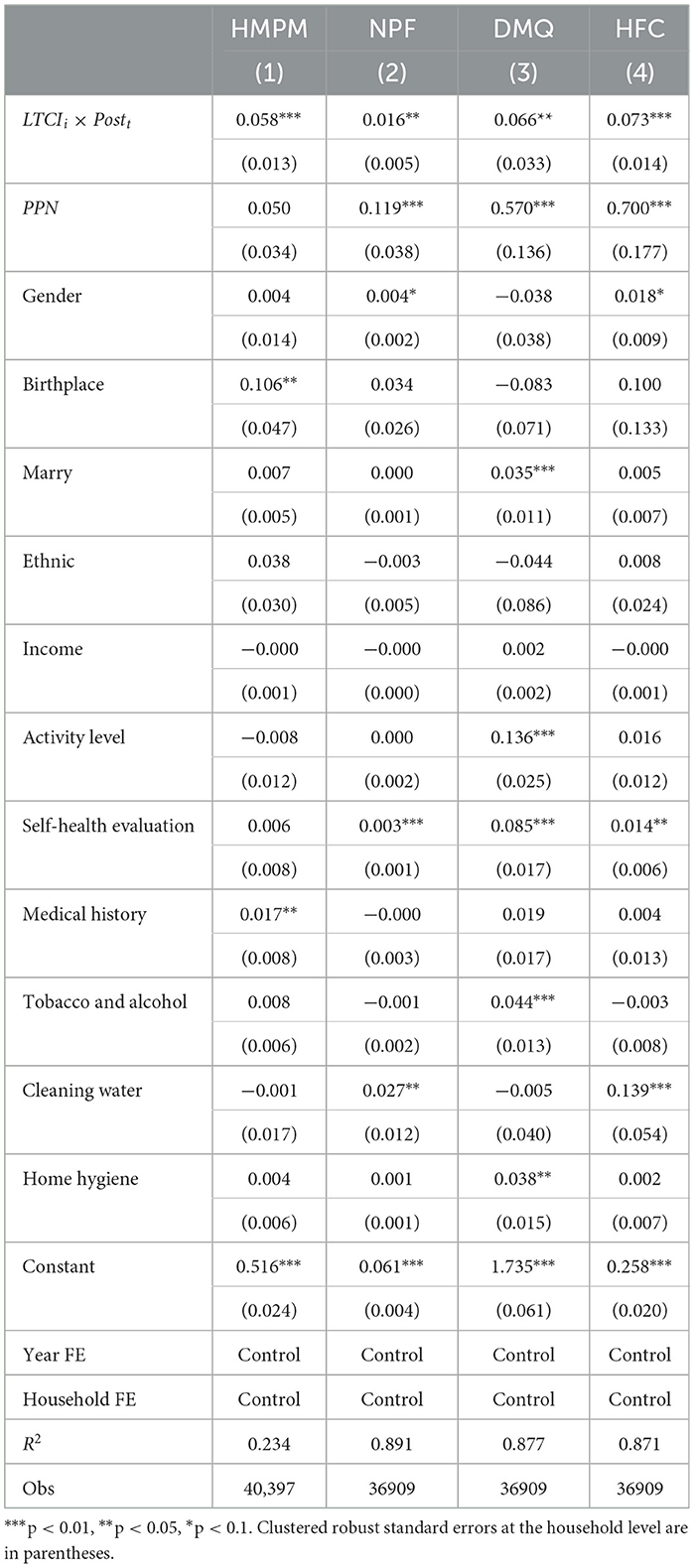
Table 7. A test of competitive policy: excluding the impact of pharmaceutical price negotiations.
5.4 Discussion of heterogeneity
Figure 3 shows the difference in the impact of LTCI policies between urban and rural areas. The LTCI policy can better promote healthy food consumption among urban families. Generally, urban families have relatively higher income levels and better economic conditions (Min et al., 2021). LTCI policies can help urban families share the financial burden of caring for sick family members and reduce financial pressure. This leaves urban households with more funds to spend on healthy food. In addition, urban residents generally pay more attention to health and quality of life. LTCI policies can remind people to pay attention to the health problems of family members and strengthen attention and emphasis on health. Urban households are more likely to be aware of the importance of food to health and are more inclined to purchase healthy foods. Urban areas generally have more healthy food supply channels, such as organic food stores, health supermarkets, etc. Implementing LTCI will likely promote the development of healthy food markets in urban areas further, providing a greater variety and better quality of healthy food options. Relative to rural areas, urban households prefer a convenient and fast lifestyle. LTCI policies can reduce the burden of caring for family members, allowing family members to spend more time and energy purchasing, preparing, and enjoying healthy foods. However, rural families may face financial challenges, especially after paying for long-term care, and they may not easily afford more expensive healthy food expenditures. Even if LTCI policies bring some economic support, this does not necessarily translate into more healthy food consumption. Moreover, rural households may be more inclined to spend their limited economic resources on obtaining primary health care services rather than purchasing more expensive healthy foods.
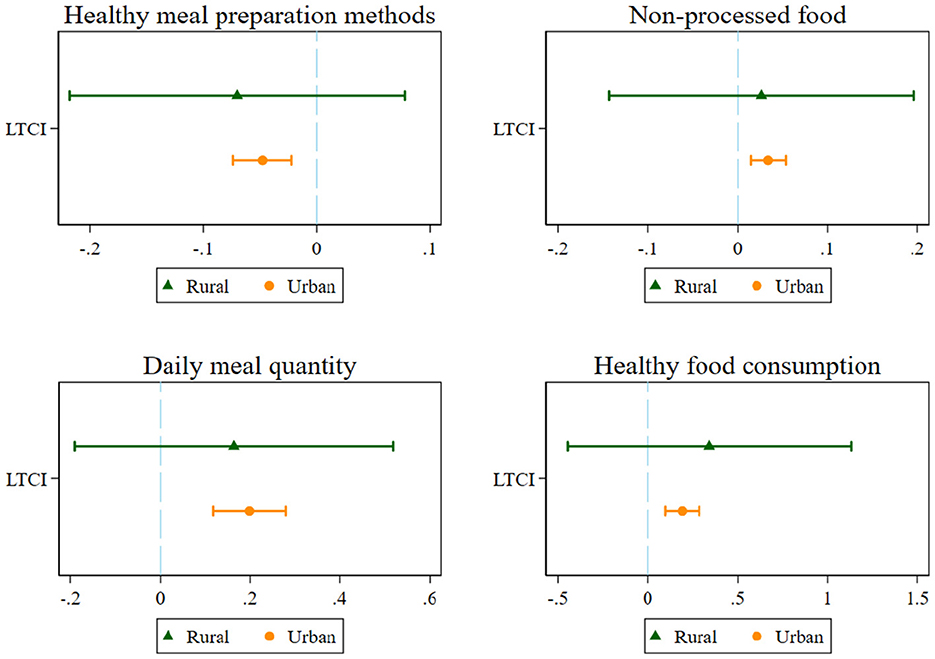
Figure 3. Urban-rural heterogeneity estimation results.
Differences in household size also have heterogeneous effects. This study will conduct group estimates based on the number of family members. Those with ≤ 2 family members form a group, and those with more than two form a group. Figure 4 shows that LTCI policies can promote healthy food consumption among larger households. The opposite behavior occurs only in healthy meal preparation methods. Generally speaking, a family with more people needs more food, and its economic expenditure is relatively higher. The LTCI policy can provide these families with financial support and help them bear higher food expenditures. Therefore, these households may be more likely to purchase healthier foods to ensure the nutritional needs of family members (Liu C. et al., 2021). Moreover, in larger families, there may be elderly or sick members who require long-term care. Long-term care insurance policies can provide these families with necessary care services and support, including dietary adjustments, nutritional supplements, etc. (Steeves et al., 2020). In this case, family members are likelier to choose healthy foods to meet caregiving needs. In larger households, family members may pay attention to each other and influence food choices (Liu C. et al., 2021). When the number of people is small, the LTCI policy increases healthy meal preparation methods. This may be related to the convenience of healthy meal preparation methods. With a small number of people, they will spend less time on complicated cooking methods. Additionally, smaller families may face more significant financial pressure because they cannot achieve the same savings in food costs as larger families through economies of scale (Deaton and Paxson, 1998). Moreover, smaller families may be more limited and inclined to spend their limited economic resources on basic living rather than purchasing more expensive healthy foods. LTCI policy does not directly address families’ food expenditures. Finally, food storage and waste may be a bigger problem for smaller families, as they may not be able to effectively take advantage of buying food in bulk. Therefore, smaller families will not increase their food expenditures much.
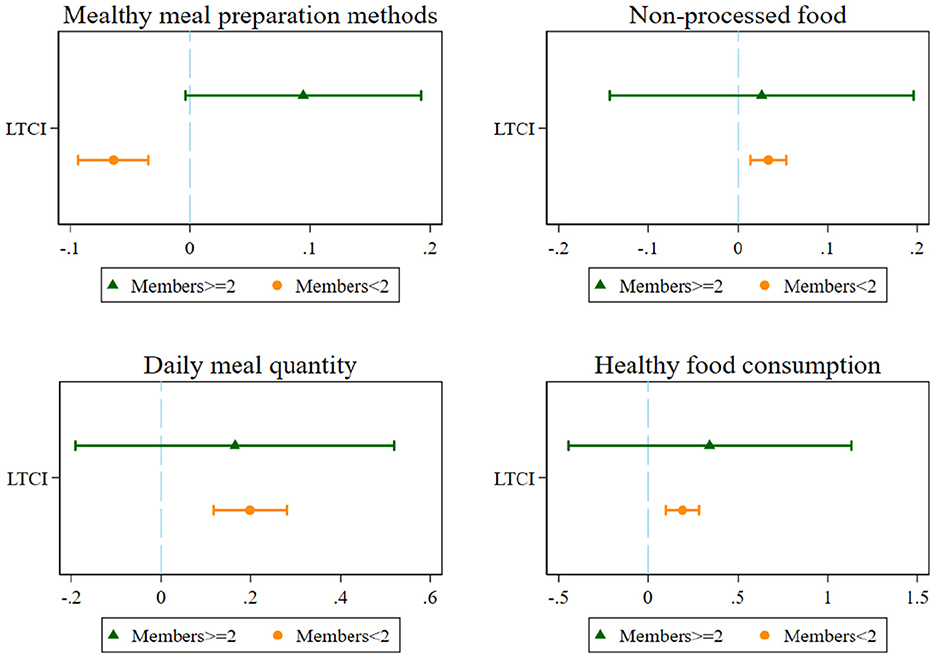
Figure 4. Family size heterogeneity estimation results.
The nature of a household member’s work unit may also be an essential factor influencing healthy food consumption. This study will use group estimates based on the categories of family members’ work units according to CHNS statistics. We divide the work units into government agencies, state-owned institutions, research institutes, state-owned enterprises, and collective enterprises into the state-owned unit group (SOE), and the rest are classified into the private enterprise group (Non-SOE). The results in Figure 5 show that different unit categories will affect the effect of the LTCI policy on healthy food consumption. Among them, the LTCI policy is more able to promote healthy food consumption among households working in private enterprises. Families working in private enterprises usually do not have stable job security and generous benefits like those in state-owned enterprises (Ma et al., 2023a), so they pay more attention to their health and welfare than their families. In this case, an LTCI policy can provide them with financial support to cope with the long-term illness and care needs that family members may face, thereby alleviating their financial pressure. This reduced financial stress can make them more likely to purchase more healthy foods to keep their families healthy. On the contrary, families working in state-owned enterprises usually have relatively stable job security and better welfare benefits (Serrano-Alarcón et al., 2022; Ma et al., 2023a), so they may pay more attention to other aspects of consumption, such as travel or entertainment. At the same time, the welfare benefits in state-owned enterprises are usually more generous than those in private enterprises, and they may pay less attention to the financial support provided by LTCI policies. On top of that, cultural and social factors further shape consumer behavior in these contexts (Wang et al., 2021). In the private sector, cultural values emphasizing individualism, materialism, and consumerism may drive higher consumption levels as individuals seek to express their identity and status through purchases. Social factors such as peer influence, media advertising, and lifestyle aspirations can also play an essential role in shaping consumption patterns in the private sector. In contrast, in state-owned enterprises, cultural values of collectivism, frugality, and social harmony may lead to more restrained consumption behavior (Bian et al., 2023). Social factors such as government campaigns to promote frugality, community norms emphasizing modesty, and concerns about sustainable resource use may influence individuals to prioritize the greater good over personal desires, leading to more conservative consumption choices.
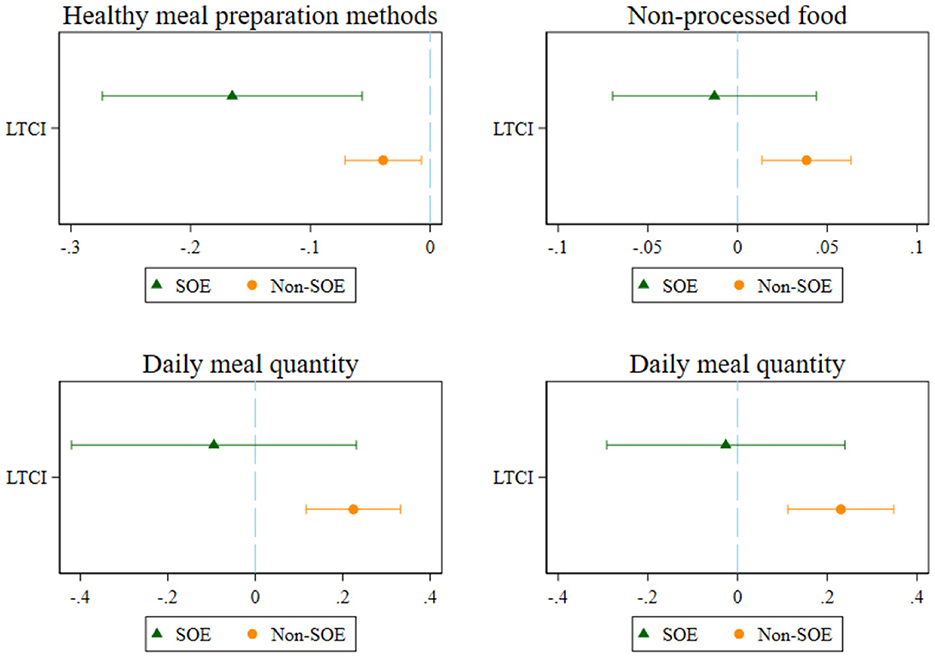
Figure 5. Work unit type heterogeneity estimation results.
6 Conclusions and implications
6.1 Conclusions
This study focuses on LTCI policies closely related to health consumption. We used CHNS data from 1989 to 2015 and adopted the DID analysis framework to examine the impact of changes in consumption behavior on healthy food consumption after households participated in the LTCI pilot. The results show that participation in LTCI policies can effectively increase healthy food consumption among Chinese households. This conclusion remains robust after parallel trend testing, placebo testing, and changing estimation methods. This conclusion adds to the existing literature on the impact of LTCI policies on healthy food consumption. Serrano-Alarcón et al. (2022) studied the impact of LTCI policy on household consumption and savings of the elderly. Recent literature discusses the effects of China’s LTCI policy on household health consumption (Liu et al., 2023). However, many health food consumption-related issues regarding LTCI policy have not been well-discussed. These issues are essential for public health and wellbeing and understanding healthy food consumption preferences in consumer behavior. Our findings thus complement the missing literature on this point. Mechanism test shows that LTCI increases families’ healthy diet preparation methods, daily meal consumption, and healthy food consumption structure through risk prevention mechanisms. After controlling for the Free Medical Examination Program and Pharmaceutical Price Negotiations, the estimated coefficients of LTCI are still significantly positive, indicating to a certain extent that the LTCI policy still has a robust effect on increasing healthy food consumption. The heterogeneity test further proves that the LTCI policy can promote healthy food consumption among urban households. LTCI policies can also better promote healthy food consumption among larger households. Moreover, it is more likely to promote healthy food consumption among households working in the private sector.
6.2 Policy implications
The findings of this study have specific policy implications and practical significance for improving public health and increasing residents’ healthy food consumption. First, carrying out LTCI can improve the preventive and rehabilitation care system from the social level, transform the public’s medical needs into nursing needs, reduce unnecessary excessive medical treatment, and promote a daily healthy diet. The government should increase the publicity of LTCI, improve public awareness and understanding of LTCI, and encourage families to participate in LTCI to reduce the financial pressure faced by families due to illness and care needs while increasing the demand and consumption of healthy foods.
Secondly, the government should strengthen the popularization of healthy food knowledge among consumers and improve consumers’ awareness and understanding of healthy food through publicity and education to better understand the importance of healthy food to physical health. Especially in rural areas, it is necessary to build healthy food supply channels, such as organic food stores, health supermarkets, etc.
Finally, the study’s findings provide insights into specific factors that influence public health outcomes, such as access to health care, social determinants of health, and the impact of public health interventions. Policymakers can use this information to allocate resources more effectively, address the root causes of health disparities, and promote equitable access to health care. Additionally, findings may highlight the need for cross-sector collaboration and the integration of health considerations into non-health policies. Policymakers should work in areas as diverse as education, urban and rural planning, and economic development to develop holistic public health approaches that address the broader determinants of wellbeing.
6.3 Limitations
This study analyzes the relationship between consumer behavior and healthy food consumption, considering differences in demographic characteristics, socioeconomic status, and individual health levels. Nonetheless, this study has some limitations. Limited by data availability and the short duration of the LTCI pilot, only four provinces served as the experimental group in this study. Moreover, the geographical information of CHNS only reaches the provincial level. However, this study uses a variety of robustness tests, including weighting, to determine the credibility of the main results. However, this study cannot further analyze specific pilot cities or more detailed districts and counties. As time passes, more and more cities have begun pilot work on long-term care insurance, and more and more research databases have opened special questionnaires on LTCI. More high-quality empirical research on LTCI policies is expected in the future. Furthermore, future research should focus on assessing the scalability and sustainability of LTCI policies. Such research can help policymakers determine how to effectively implement and sustain LTCI policy interventions on a larger scale and ensure that LTCI has a positive and sustained impact on public health outcomes.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
WC: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. GM: Conceptualization, Data curation, Formal analysis, Methodology, Supervision, Writing – original draft, Writing – review & editing. ZJ: Formal analysis, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Shanghai Philosophy and Social Sciences Planning Project (Grant No. 2021BJB003) and the Fundamental Research Funds for the Central Universities (Grant No. CXJJ-2023-430).
Acknowledgments
The authors thank Dr. Yumeng Zhang from the School of Economics and Management, Nanjing Vocational University of Industry Technology, and Professor Xin Li from the College of Business and Economics, Shanghai Business School, for their help in writing the article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abadie, A. (2005). Semiparametric difference-in-differences estimators. Rev. Econ. Stud. 72, 1–19. doi: 10.1111/0034-6527.00321
Crossref Full Text | Google Scholar
Ameriks, J., Briggs, J., Caplin, A., Shapiro, M. D., and Tonetti, C. (2020). Long-term-care utility and late-in-life saving. J. Polit. Econ. 128, 2375–2451. doi: 10.1086/706686
Crossref Full Text | Google Scholar
Bai, Y., Alemu, R., Block, S. A., Headey, D., and Masters, W. A. (2021). Cost and affordability of nutritious diets at retail prices: evidence from 177 countries. Food Policy 99:101983. doi: 10.1016/j.foodpol.2020.101983
PubMed Abstract | Crossref Full Text | Google Scholar
Bertrand, M., Duflo, E., and Mullainathan, S. (2004). How much should we trust differences-in-differences estimates? Q. J. Econ. 119, 249–275. doi: 10.1162/003355304772839588
Crossref Full Text | Google Scholar
Bian, H., Jin, F., and Tong, X. (2023). Carbon reduction consciousness, determinants and value of low-carbon transition: evidence from textual and empirical analysis of chinese listed manufacturing enterprises. Int. Rev. Econ. Finan. 88, 1301–1323. doi: 10.1016/j.iref.2023.07.061
Crossref Full Text | Google Scholar
Boyland, E. J., Nolan, S., Kelly, B., Tudur-Smith, C., Jones, A., Halford, J. C., et al. (2016). Advertising as a cue to consume: a systematic review and meta-analysis of the effects of acute exposure to unhealthy food and nonalcoholic beverage advertising on intake in children and adults12. Am. J. Clin. Nutr. 103, 519–533. doi: 10.3945/ajcn.115.120022
PubMed Abstract | Crossref Full Text | Google Scholar
Bronchetti, E. T. (2012). Workers’ compensation and consumption smoothing. J. Public Econ. 96, 495–508. doi: 10.1016/j.jpubeco.2011.12.005
Crossref Full Text | Google Scholar
Caso, D., Guidetti, M., Capasso, M., and Cavazza, N. (2022). Finally, the chance to eat healthily: longitudinal study about food consumption during and after the first COVID-19 lockdown in Italy. Food Qual. Prefer. 95:104275. doi: 10.1016/j.foodqual.2021.104275
PubMed Abstract | Crossref Full Text | Google Scholar
Chen, F., Zhang, X., and Chen, Z. (2023). Air pollution and mental health: evidence from China Health and Nutrition Survey. J. Asian Econ. 86:101611. doi: 10.1016/j.asieco.2023.101611
Crossref Full Text | Google Scholar
Deaton, A., and Paxson, C. (1998). Economies of scale, household size, and the demand for food. J. Polit. Econ. 106, 897–930. doi: 10.1086/250035
Crossref Full Text | Google Scholar
Ding, Y., Min, S., Wang, X., and Yu, X. (2022). Memory of famine: the persistent impact of famine experience on food waste behavior. China Econ. Rev. 73:101795. doi: 10.1016/j.chieco.2022.101795
Crossref Full Text | Google Scholar
Dominguez-Viera, M. E., van den Berg, M., Donovan, J., Perez-Luna, M. E., Ospina-Rojas, D., and Handgraaf, M. (2022). Demand for healthier and higher-priced processed foods in low-income communities: experimental evidence from Mexico city. Food Qual. Prefer. 95:104362. doi: 10.1016/j.foodqual.2021.104362
Crossref Full Text | Google Scholar
Eyinade, G. A., Mushunje, A., and Yusuf, S. F. G. (2021). The willingness to consume organic food: a review. Food Agric. Immunol. 32, 78–104. doi: 10.1080/09540105.2021.1874885
Crossref Full Text | Google Scholar
Fang, F., Zhao, Y., Xi, Z., Han, X., and Zhu, Y. (2023). The impact of famine experience on middle-aged and elderly individuals’ food consumption: evidence from China. J. Econ. Ageing 26:100472. doi: 10.1016/j.jeoa.2023.100472
Crossref Full Text | Google Scholar
Feng, J., Wang, Z., and Yu, Y. (2020). Does long-term care insurance reduce hospital utilization and medical expenditures? Evidence from China. Soc. Sci. Med. 258:113081. doi: 10.1016/j.socscimed.2020.113081
PubMed Abstract | Crossref Full Text | Google Scholar
Feng, Z., Glinskaya, E., Chen, H., Gong, S., Qiu, Y., Xu, J., et al. (2020). Long-term care system for older adults in China: policy landscape, challenges, and future prospects. Lancet 396, 1362–1372. doi: 10.1016/S0140-6736(20)32136-X
PubMed Abstract | Crossref Full Text | Google Scholar
Fu, R., Noguchi, H., Kawamura, A., Takahashi, H., and Tamiya, N. (2017). Spillover effect of Japanese long-term care insurance as an employment promotion policy for family caregivers. J. Health Econ. 56, 103–112. doi: 10.1016/j.jhealeco.2017.09.011
PubMed Abstract | Crossref Full Text | Google Scholar
Ghufran, M., Ali, S., Ariyesti, F. R., Nawaz, M. A., Aldieri, L., and Xiaobao, P. (2022). Impact of Covid-19 to customers switching intention in the food segments: the push, pull and mooring effects in consumer migration towards organic food. Food Qual. Prefer. 99:104561. doi: 10.1016/j.foodqual.2022.104561
Crossref Full Text | Google Scholar
Goossensen, M., Garcia, X., Garcia-Sierra, M., Calvet-Mir, L., and Domene, E. (2023). The role of convenience stores in healthy food environments: the case of Barcelona (Spain). Cities 133:104118. doi: 10.1016/j.cities.2022.104118
Crossref Full Text | Google Scholar
Haq, S.u, Shahbaz, P., Abbas, A., Alhafi Alotaibi, B., Nadeem, N., et al. (2023). Looking up and going down: does sustainable adaptation to climate change ensure dietary diversity and food security among rural communities or vice versa? Front. Sustain. Food Syst. 7:1142826. doi: 10.3389/fsufs.2023.1142826
Crossref Full Text | Google Scholar
Houngbedji, K. (2016). Abadie’s semiparametric difference-in-differences estimator. Stata J. 16, 482–490. doi: 10.1177/1536867X1601600213
Crossref Full Text | Google Scholar
Imrohoroǧlu, A., and Zhao, K. (2018). The Chinese saving rate: long-term care risks, family insurance, and demographics. J. Monet. Econ. 96, 33–52. doi: 10.1016/j.jmoneco.2018.03.001
PubMed Abstract | Crossref Full Text | Google Scholar
Kennedy, G., Ahern, M. B., Iannotti, L. L., Vie, S., Sherburne, L., and Thilsted, S. H. (2023). Considering the food environment can help to promote the consumption of aquatic foods for healthy diets. Front. Sustain. Food Syst. 7:1241548. doi: 10.3389/fsufs.2023.1241548
Crossref Full Text | Google Scholar
Kopecky, K. A., and Koreshkova, T. (2014). The impact of medical and nursing home expenses on savings. Am. Econ. J. Macroecon. 6, 29–72. doi: 10.1257/mac.6.3.29
Crossref Full Text | Google Scholar
Lachowska, M., and Myck, M. (2018). The effect of public pension wealth on saving and expenditure. Am. Econ. J. 10, 284–308. doi: 10.1257/pol.20150154
Crossref Full Text | Google Scholar
Le, T. P., DeJesus-Rodriguez, A., Rihal, T. K., and Raposa, E. B. (2023). Associations between trait food craving and adolescents’ preferences for and consumption of healthy versus unhealthy foods. Food Qual. Prefer. 108:104887. doi: 10.1016/j.foodqual.2023.104887
Crossref Full Text | Google Scholar
Lee, H.-J., and Yun, Z.-S. (2015). Consumers’ perceptions of organic food attributes and cognitive and affective attitudes as determinants of their purchase intentions toward organic food. Food Qual. Prefer. 39, 259–267. doi: 10.1016/j.foodqual.2014.06.002
Crossref Full Text | Google Scholar
Lei, X., Bai, C., Hong, J., and Liu, H. (2022). Long-term care insurance and the well-being of older adults and their families: evidence from China. Soc. Sci. Med. 296:114745. doi: 10.1016/j.socscimed.2022.114745
PubMed Abstract | Crossref Full Text | Google Scholar
Lian, T., Haq, S. U., Shahbaz, P., Zhao, L., Nadeem, M., and Aziz, B. (2023). Changing food patterns during the pandemic: exploring the role of household dynamics and income stabilization strategies. Sustainability 15:123. doi: 10.3390/su15010123
Crossref Full Text | Google Scholar
Liu, C., Yi, F., Xu, Z., and Tian, X. (2021). Do living arrangements matter?—evidence from eating behaviors of the elderly in rural China. J. Econ. Ageing 19:100307. doi: 10.1016/j.jeoa.2021.100307
Crossref Full Text | Google Scholar
Liu, H., and Hu, T. (2022). Evaluating the long-term care insurance policy from medical expenses and health security equity perspective: evidence from China. Arch. Public Health 80:1. doi: 10.1186/s13690-021-00761-7
PubMed Abstract | Crossref Full Text | Google Scholar
Liu, H., Ma, J., and Zhao, L. (2023). Public long-term care insurance and consumption of elderly households: evidence from China. J. Health Econ. 90:102759. doi: 10.1016/j.jhealeco.2023.102759
PubMed Abstract | Crossref Full Text | Google Scholar
Liu, Q., and Lu, Y. (2015). Firm investment and exporting: evidence from China’s value-added tax reform. J. Int. Econ. 97, 392–403. doi: 10.1016/j.jinteco.2015.07.003
Crossref Full Text | Google Scholar
Liu, Y., Diao, L., and Xu, L. (2021). The impact of childhood experience of starvations on the health of older adults: evidence from China. Int. J. Health Plann. Manage. 36, 515–531. doi: 10.1002/hpm.3099
PubMed Abstract | Crossref Full Text | Google Scholar
Ljubičić, M., Matek Sarić, M., Klarin, I., Rumbak, I., Colić Barić, I., Ranilović, J., et al. (2023). Emotions and food consumption: emotional eating behavior in a European population. Foods 12:12040872. doi: 10.3390/foods12040872
PubMed Abstract | Crossref Full Text | Google Scholar
Luo, Y., Min, S., and Bai, J. (2021). The role of rubber farming in household dietary diversity in the upper Mekong region, Southwest China. Food Energy Sec. 10:e285. doi: 10.1002/fes3.285
Crossref Full Text | Google Scholar
Luo, Y., Yuan, K., Li, Y., Liu, Y., and Pan, Y. (2024). The “spillover effect” of long-term care insurance in china on spouses’ health and well-being. Soc. Sci. Med. 340:116487. doi: 10.1016/j.socscimed.2023.116487
PubMed Abstract | Crossref Full Text | Google Scholar
Ma, G., Cao, J., and Famanta, M. (2023a). Does the coordinated development of two-way FDI increase the green energy efficiency of Chinese cities? Evidence from Chinese listed companies. Struct. Change Econ. Dyn. 65, 59–77. doi: 10.1016/j.strueco.2023.02.007
Crossref Full Text | Google Scholar
Ma, G., Qin, J., and Zhang, Y. (2023b). Does the carbon emissions trading system reduce carbon emissions by promoting two-way FDI in developing countries? Evidence from Chinese listed companies and cities. Energy Econ. 120:106581. doi: 10.1016/j.eneco.2023.106581
Crossref Full Text | Google Scholar
Min, S., Wang, X., and Yu, X. (2021). Does dietary knowledge affect household food waste in the developing economy of China? Food Policy 98:101896. doi: 10.1016/j.foodpol.2020.101896
PubMed Abstract | Crossref Full Text | Google Scholar
Parashar, S., Singh, S., and Sood, G. (2023). Examining the role of health consciousness, environmental awareness and intention on purchase of organic food: a moderated model of attitude. J. Clean. Prod. 386:135553. doi: 10.1016/j.jclepro.2022.135553
Crossref Full Text | Google Scholar
Royo-Bordonada, M., León-Flández, K., Damián, J., Bosqued-Estefanía, M., Moya-Geromini, M., and López-Jurado, L. (2016). The extent and nature of food advertising to children on Spanish television in 2012 using an international food-based coding system and the uk nutrient profiling model. Public Health 137, 88–94. doi: 10.1016/j.puhe.2016.03.001
PubMed Abstract | Crossref Full Text | Google Scholar
Serrano-Alarcón, M., Hernández-Pizarro, H., López-Casasnovas, G., and Nicodemo, C. (2022). Effects of long-term care benefits on healthcare utilization in Catalonia. J. Health Econ. 84:102645. doi: 10.1016/j.jhealeco.2022.102645
PubMed Abstract | Crossref Full Text | Google Scholar
Shahbaz, P., ul Haq, S., Abbas, A., Samie, A., Boz, I., Bagadeem, S., et al. (2022). Food, energy, and water nexus at household level: do sustainable household consumption practices promote cleaner environment? Int. J. Environ. Res. Public Health 19:12945. doi: 10.3390/ijerph191912945
PubMed Abstract | Crossref Full Text | Google Scholar
Shahzad, M. A., Qing, P., Rizwan, M., Razzaq, A., and Faisal, M. (2021). Covid-19 pandemic, determinants of food insecurity, and household mitigation measures: a case study of Punjab, Pakistan. Healthcare 9:621. doi: 10.3390/healthcare9060621
PubMed Abstract | Crossref Full Text | Google Scholar
Shahzad, M. A., Razzaq, A., Qing, P., Rizwan, M., and Faisal, M. (2022). Food availability and shopping channels during the disasters: has the Covid-19 pandemic changed peoples’ online food purchasing behavior? Int. J. Disast. Risk Reduct. 83:103443. doi: 10.1016/j.ijdrr.2022.103443
PubMed Abstract | Crossref Full Text | Google Scholar
Shahzad, M. A., Wang, L., Qin, S., and Zhou, S. (2023). Covid-19 incidence of poverty: how has disease affected the cost of purchasing food in Pakistan. Prev. Med. Rep. 36:102477. doi: 10.1016/j.pmedr.2023.102477
PubMed Abstract | Crossref Full Text | Google Scholar
Sim, A. Y., and Cheon, B. K. (2019). Influence of impending healthy food consumption on snacking: Nudging vs. compensatory behaviour. Physiol. Behav. 198, 48–56. doi: 10.1016/j.physbeh.2018.10.010
PubMed Abstract | Crossref Full Text | Google Scholar
Solbak, N. M., Xu, J.-Y., Vena, J. E., Csizmadi, I., Whelan, H. K., and Robson, P. J. (2017). Diet quality is associated with reduced incidence of cancer and self-reported chronic disease: observations from Alberta’s tomorrow project. Prev. Med. 101, 178–187. doi: 10.1016/j.ypmed.2017.06.009
PubMed Abstract | Crossref Full Text | Google Scholar
Steeves, S., Acciai, F., Tasevska, N., DeWeese, R. S., Yedidia, M. J., and Ohri-Vachaspati, P. (2020). The special supplemental nutrition program for women, infants, and children spillover effect: do siblings reap the benefits? J. Acad. Nutr. Diet. 120, 1288–1294. doi: 10.1016/j.jand.2020.02.013
PubMed Abstract | Crossref Full Text | Google Scholar
Sun, D., Liu, Y., Grant, J., Long, Y., Wang, X., and Xie, C. (2021). Impact of food safety regulations on agricultural trade: evidence from China’s import refusal data. Food Policy 105:102185. doi: 10.1016/j.foodpol.2021.102185
Crossref Full Text | Google Scholar
Wang, H., Guo, T., and Tang, Q. (2021). The effect of national culture on corporate green proactivity. J. Bus. Res. 131, 140–150. doi: 10.1016/j.jbusres.2021.03.023
Crossref Full Text | Google Scholar
Wang, Z., and Li, K. (2023). Can environmentally themed music increase consumers’ willingness to pay for low-carbon food? A discrete choice experiment method. Front. Sustain. Food Syst. 7:1302511. doi: 10.3389/fsufs.2023.1302511
Crossref Full Text | Google Scholar
Werthmann, J., Tuschen-Caffier, B., Ströbele, L., Kübel, S. L., and Renner, F. (2023). Healthy cravings? Impact of imagined healthy food consumption on craving for healthy foods and motivation to eat healthily – results of an initial experimental study. Appetite 183:106458. doi: 10.1016/j.appet.2023.106458
PubMed Abstract | Crossref Full Text | Google Scholar
Xu, H., Xiao, M., Zeng, J., and Hao, H. (2023). Green-labelled rice versus conventional rice: perception and emotion of Chinese consumers based on review mining. Foods 12:12010087. doi: 10.3390/foods12010087
PubMed Abstract | Crossref Full Text | Google Scholar
Xu, X., Hall, J., Byles, J., and Shi, Z. (2015). Dietary pattern is associated with obesity in older people in china: data from China Health and Nutrition Survey (CHNS). Nutrients 7, 8170–8188. doi: 10.3390/nu7095386
PubMed Abstract | Crossref Full Text | Google Scholar
Yang, Q., Al Mamun, A., Naznen, F., Siyu, L., and Mohamed Makhbul, Z. K. (2023). Modelling the significance of health values, beliefs and norms on the intention to consume and the consumption of organic foods. Heliyon 9:e17487. doi: 10.1016/j.heliyon.2023.e17487
PubMed Abstract | Crossref Full Text | Google Scholar
Yang, Y., and Ma, G. (2023). How can hsr promote inter-city collaborative innovation across regional borders? Cities 138:104367. doi: 10.1016/j.cities.2023.104367
Crossref Full Text | Google Scholar
Zhu, Q., Li, Y., Geng, Y., and Qi, Y. (2013). Green food consumption intention, behaviors and influencing factors among Chinese consumers. Food Qual. Prefer. 28, 279–286. doi: 10.1016/j.foodqual.2012.10.005
Crossref Full Text | Google Scholar
Zhu, Y., and Österle, A. (2017). Rural-urban disparities in unmet long-term care needs in China: the role of the Hukou status. Soc. Sci. Med. 191, 30–37. doi: 10.1016/j.socscimed.2017.08.025
PubMed Abstract | Crossref Full Text | Google Scholar