Introduction
Binge eating (consuming an objectively large amount of food while feeling a loss of control) is a core component of bulimia nervosa (BN). Although loss of control may be more important than the amount of food consumed in understanding distress related to binge eating (Latner et al., 2007), people with BN have recurrent objectively large binge eating episodes by definition (APA, 2013), and consideration of binge size may help inform understanding of BN (Mourilhe et al., 2021).
Accumulating evidence suggests binge size is an important marker of distress and impairment, particularly within BN. A recent meta-analysis found that caloric intake during binge eating episodes was positively correlated with depressive symptoms in BN (Mourilhe et al., 2021). Greater binge size also is associated with lower quality of life, higher weight/shape concerns, elevated anxiety symptoms, greater weight suppression, and more eating disorder impairment (Forney et al., 2016; Keel et al., 2019; Li et al., 2019; Bruzas et al., 2022). As such, further investigation into the predictors of binge size is warranted. Dispositional traits may be associated with greater binge size. If so, such traits may be targeted in BN interventions.
One set of dispositional traits that merit consideration are negative urgency (NU) and positive urgency (PU). NU refers to the tendency to engage in rash behavior when experiencing negative affect (Cyders and Smith, 2008). PU is characterized by engaging in rash action when experiencing positive affect (Cyders and Smith, 2007; Cyders and Smith, 2008). Both are part of a family of five impulsigenic traits that contribute to impulsive behavior, but are only modestly correlated with each other (Whiteside and Lynam, 2001; Cyders and Smith, 2007; Smith et al., 2007). Multiple meta-analyses have established that, of the impulsigenic traits, NU and PU consistently demonstrate the largest correlations and effect sizes with many forms of impulsive behaviors, including bulimic behaviors, substance use, and suicidality (Fischer et al., 2008; Coskunpinar et al., 2013; Berg et al., 2015; Smith and Cyders, 2016). NU has been widely investigated as a risk factor for and correlate of bulimic pathology. Across studies, NU predicts the development of binge eating among adolescents (Pearson et al., 2012; Davis and Smith, 2018), is elevated in BN compared to control groups (Fischer et al., 2008) and is associated with binge eating frequency cross-sectionally and longitudinally (Fischer et al., 2018; Kenny et al., 2019). However, the association between NU and binge size has been less studied.
Although PU has been studied relatively less in relation to eating pathology than NU, and some research suggests PU may not be relevant to eating pathology (Cyders and Smith, 2007), three recent studies support potential associations between PU and binge-spectrum eating disorders. In a clinical sample, PU (but no other impulsigenic trait) was associated with non-suicidal self-injury in BN (Claes et al., 2015). In another clinical sample, PU was cross-sectionally associated with binge frequency among binge-spectrum eating disorders (Michael and Juarascio, 2021). A third study found participants with binge eating disorder reported elevated levels of PU and NU, compared to overweight and non-overweight controls, and the two traits were associated with elevated eating pathology (Kenny et al., 2019). Altogether, findings support examining the potential role of PU in BN symptom expression, including binge size.
Broadly, emotion regulation theories posit that individuals with BN attempt to manage intense affect (negative or positive–but more research focuses on negative) by engaging in binge eating (Pearson et al., 2015; Safer, 2015). Accordingly, NU and PU may prompt binge eating in BN. Emotional intensity is thought to decrease following binge eating, thus providing negative reinforcement (Pearson et al., 2015; Safer, 2015). Importantly, NU and PU each correlate with emotion dysregulation in cross-sectional and longitudinal studies (King et al., 2018; Feil et al., 2020), suggesting they reflect dispositional challenges with responding to affect.
Despite the historical focus on negative emotion regulation (Pearson et al., 2015) and findings demonstrating decreases in positive affect prior to binge eating (Schaefer et al., 2020), there is emerging concern regarding the potentially important role of positive emotion dysregulation in eating disorders (Selby et al., 2019). Theory underlying associations between PU and binge eating is limited, but it may be that individuals high in PU experience positive, rather than negative, reinforcement from binge eating, given high levels of dispositional positive affect (e.g., excitement) and the inherent rewarding properties of palatable foods often consumed while binge eating (de Macedo et al., 2016). For example, eating a large amount of cake at a party may provide positive reinforcement in the form of mood enhancement. Indeed, theory posits rash action while feeling strong positive emotions provides positive reinforcement by enhancing a celebratory mood (Cyders and Smith, 2008) and positive affect has been shown to increase following binge eating (Wonderlich et al., 2018; Schaefer et al., 2020). Further, individuals who binge eat report eating when they feel especially good (Johnson et al., 1995). In contrast, individuals higher in NU (versus PU) may be more prone to negative reinforcement from binge eating.
It is thus possible that elevations in NU and PU contribute to not only risk for binge eating (Davis and Smith, 2018) but also binge size. Few studies have tested associations between urgency and binge size. Forney et al. (2016) found that NU was not associated with binge size among women with BN, but they did not examine potential associations with PU. Also, because binge size in this study was self-reported, it is unclear if or how NU may predict binge size measured objectively.
The current investigation sought to evaluate preliminary associations between the urgency traits and binge size using a laboratory ad lib test meal investigation. Because binge eating has been modeled in the laboratory when certain instructions are provided and individuals with BN indicate their laboratory behavior mirrors their binge eating elsewhere, laboratory episodes can provide an acceptable analog to real-life binge eating (Mitchell et al., 1998; Sysko et al., 2018). To our knowledge, no previous study has examined NU or PU in relation to binge size in the laboratory. Based on previous research (Fischer et al., 2008; Kenny et al., 2019), we sought to replicate the finding that women with BN report higher levels of NU and PU than controls. Our core hypothesis was that NU and PU would predict greater caloric consumption (larger binge size), during the ad lib test meal for women with BN, but not controls. Given high conceptual and empirical overlap between NU and PU (Cyders and Smith, 2007) we included both in the same model. Because NU and PU correlate with negative and positive affect, respectively, and higher negative affect is associated with binge eating risk (Smith et al., 2020) we included both in the model to control for the potential influence of dispositional tendencies to feel negative or positive affect in the absence of urgency.
Methods
Participants
Data come from a larger study of affective consequences of binge eating (Davis et al., 2022). Women (N = 50) were recruited from a large, public university in the southeastern United States and the community to fill two groups: a BN group that met DSM-5 criteria for BN (N = 21) and a healthy control group (N = 29). Eligibility criteria were modeled after previous ad lib test meal studies (Keel et al., 2018). Advertisements on social media and in the community invited normal-weight women with no eating concerns and women who binge ate and used weight control methods to contact the research team. Eligibility criteria were verified by telephone screen conducted by a research assistant under the supervision of a licensed psychologist. Bulimic behavior questions from the Eating Disorder Examination (Cooper and Fairburn, 1987) were used to confirm study group. Participants were required to be 18–25 years old and have a body mass index (BMI) between 18.5–26.5, based on self-report and verified with objective measure.
Exclusion criteria for all participants included current medical conditions or medication use that could influence appetite, weight, or ability to safely participate, current pregnancy, or lactation. Exclusion criteria for the BN group included being in or seeking eating disorder treatment and having a lifetime history of anorexia nervosa. Control group exclusion criteria included lifetime history of eating disorder symptoms, dietary restriction within the past 8 weeks, and excessive exercise. Women with BN were required to endorse consuming at least 1,000 kcal during binge eating episodes with a loss of control. Calories consumed were calculated by a trained research assistant, using nutritional information available on the internet (Keel et al., 2018).
Participant mean (SD) age was 19.44 (1.55) years. Participants self-identified as 74% White/European American, 10% Black/African American, 8% Hispanic, 6% Asian/Pacific Islander, and 2% biracial. BN participants were significantly older than control participants [t(df) = 3.67 (48), p ps > 0.05).
Measures
Food consumption. Ad lib test meal food was weighed before and after using a food scale. Intake was calculated in grams consumed by taking the difference of the two values and then converted to calories using the gram to calorie ratio of the food.
Urgency. The UPPS-P Impulsive Behavior Scale (Lynam et al., 2006) measured PU and NU prior to the test meal. The PU subscale consists of 14 items and the NU subscale consists of 12 items. Items are rated on a 4-point Likert scale anchored at (1) Agree Strongly and (4) Disagree Strongly. An example PU item is “I tend to act without thinking when I am really excited.” An example NU item is “When I am upset, I often act without thinking.” Subscale items are averaged for a mean score. The UPPS-P urgency scales demonstrate good reliability and validity (Cyders and Smith, 2007). Internal consistency in the current study was high (NU α =0.92; PU α = 0.94).
Dispositional Affect. The Positive and Negative Affect Schedule (PANAS; Watson et al., 1988) measured dispositional negative and positive affect prior to the test meal. The PANAS consists of 20 words that describe different emotions. Participants indicated to what extent they generally felt each word using a 5-point Likert-scale anchored at (1) Very Slightly or Not at All and (5) Extremely. The negative affect scale includes 10 negative emotions; an example is “distressed.” The positive affect scale includes 10 positive emotions; an example is “proud.” Items are summed for each scale. The PANAS demonstrates high test–retest reliability and criterion validity (DePaoli and Sweeney, 2000; Serafini et al., 2016). Internal consistency in the present study was high (negative affect α = 0.89; positive affect α = 0.92).
Procedures
The study was approved by the Institutional Review Board (IRB) at the University of Kentucky (protocol #43524). Written informed consent was obtained. All ethical guidelines in the treatment of study participants and in analyzing the retrieved data were followed. Procedures included one study visit that lasted up to two hours.
Participants were provided a 200-kcal standardized breakfast (store-bought yogurt with pre-measured granola) to consume between 9 am and 9:30 am the day of their study visit. They were instructed not to consume anything else until their 2 pm study visit (Kissileff et al., 1996). When they arrived, participants were asked if they followed the instructions, to ensure they remained eligible. If still eligible, height and weight were measured and a pregnancy test was administered. Participants completed questionnaires on an iPad.
The ad lib test meal included three foods requested by participants (Raymond et al., 2007). Participants with BN were asked to report three store-bought foods they typically consumed when binge eating, and controls were asked to report three store-bought foods they enjoyed eating. Common examples of requested food were pretzels and cookies. Enough food was provided to allow for objectively large consumption: 2000 calories of each food item was placed into a bowl or plate and served at an individual place-setting (Wolfe et al., 2002). Participants also were provided an 8-ounce bottle of water. Participants were presented with the test meal and instructions were provided verbally: “Let yourself go and eat as much as you can” (Kissileff et al., 1996). Participants were left alone in the room with the food. Immediately upon finishing the test meal, participants completed questionnaires (results reported elsewhere; Davis et al., 2022).
Participants were debriefed on the purpose of the research, provided compensation in cash ($30) for community-recruited participants or course credit for student participants, and provided a mental health resource list.
Data analysis
Data were analyzed using SPSS v.28. Descriptive statistics included means for test meal consumption and scores on UPPS-P PU, UPPS-P NU, PANAS positive affect, and PANAS negative affect. Independent samples t-tests were used to compare groups on study variables.
Hierarchical linear regression was used to assess prediction of test meal consumption from group membership, UPPS-P NU and PU, PANAS traits, and the interactions of personality traits with group membership. We constructed the interaction terms as follows. Diagnostic group (BN or control) was dummy coded, with control group as the reference. PU, NU, positive affect, and negative affect were mean-centered. We then calculated the product term of group by each of the personality variables. We were then able to determine if the interaction term had incremental predictive power above and beyond the main effects for each variable. Test meal intake was specified as the outcome variable. At step one, we entered group, PU, NU, positive affect, negative affect, and age (to control for group differences in age). At step two, we entered the interaction terms: group by PU, group by NU, group by positive affect, and group by negative affect.
Results
Descriptive statistics
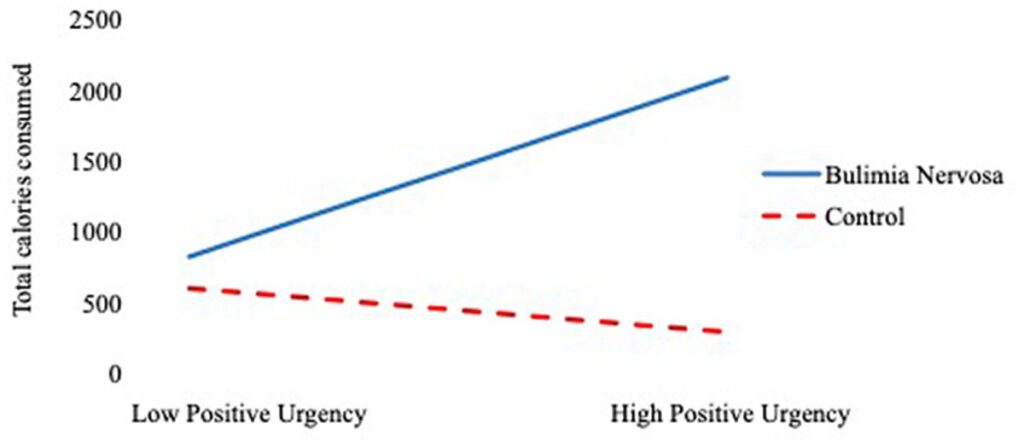
Table 1 shows descriptive statistics for test meal consumption and scores on urgency and affect by group. Table 2 presents correlations among calories consumed during test meal, NU, PU, negative affect, positive affect, and age. Women with BN consumed significantly more calories during the test meal compared with controls. In line with our first hypothesis, women with BN scored significantly higher on NU and PU compared with controls. Women with BN scored higher on negative affect, but not positive affect, compared with controls. Among the BN group, significant positive correlations were observed between total calories consumed and PU. NU and PU were positively correlated across all participants.
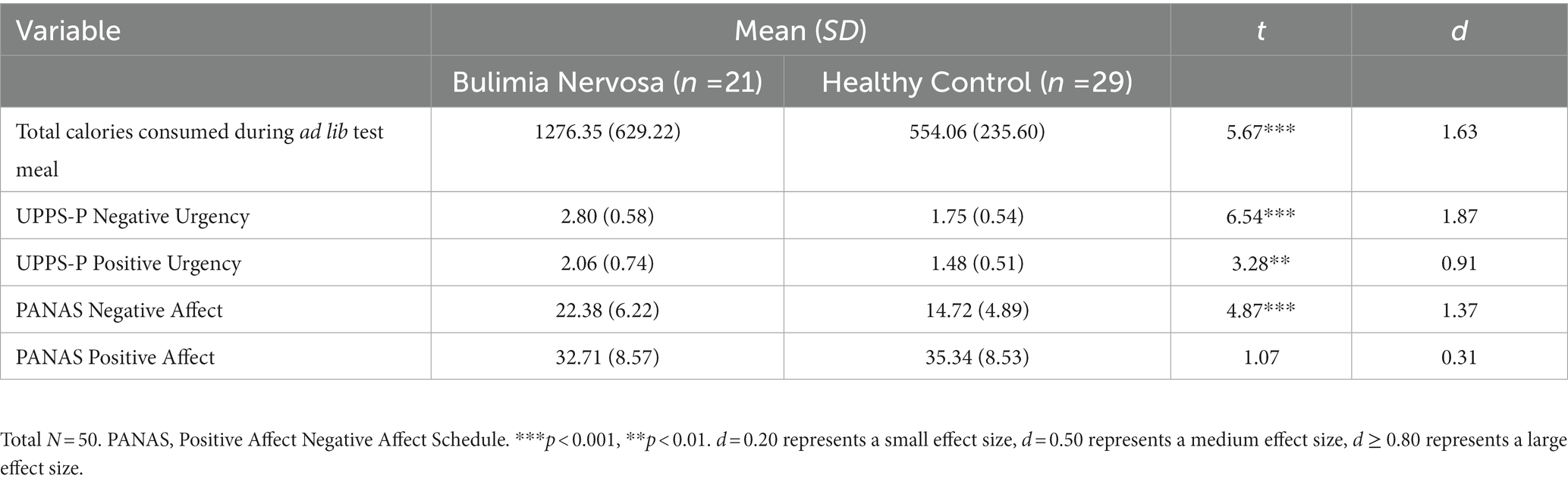
Table 1. Descriptive statistics for all study variables.
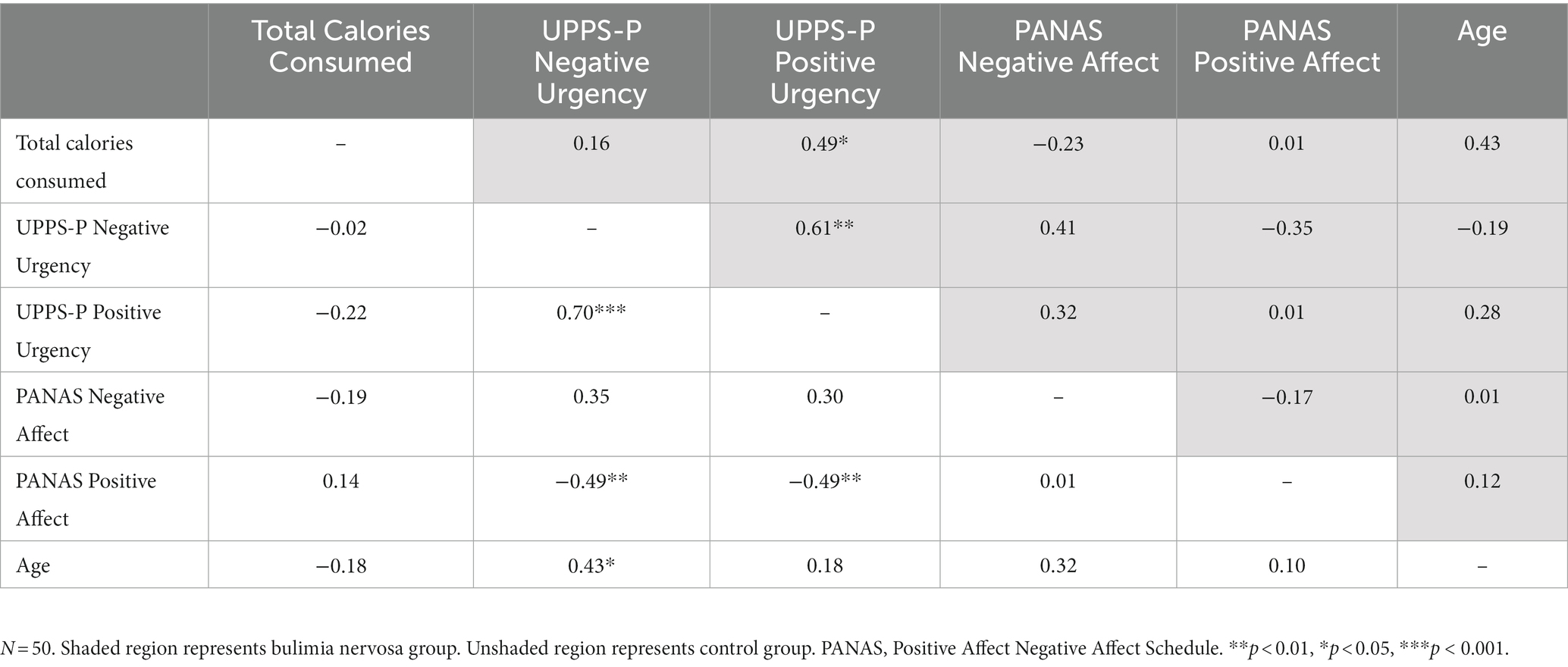
Table 2. Correlations among all study variables.
Prediction of ad lib test meal intake
Given observed correlations among study variables, we checked collinearity in the regression model by measuring variance inflation factor (VIF) values. All VIF values were under 10, indicating no problems with collinearity (Fox, 1991). Table 3 presents the regression results for the prediction of test meal intake from age, group, personality variables, and their interactions. At step 1, only group and negative affect significantly predicted ad lib test meal intake. Specifically, BN group membership predicted greater test meal intake. Negative affect level negatively predicted test meal intake across participants. There was no main effect of age, PU, NU, or positive affect on ad lib test meal intake. At Step 2, the main effect of group and the interaction of PU by group significantly predicted ad lib test meal intake. The main effects of age, PU, NU, positive affect, negative affect, and the interaction terms between group and NU, positive affect, and negative affect were not significant at Step 2. As Figure 1 shows, among participants with BN, as PU increased, caloric intake during the ad lib test meal increased. Among participants in the control group, there was not a significant relationship between PU and caloric intake during the ad lib test meal. The change in R2 from Step 1 to Step 2 was not significant, indicating no increase in incremental predictive power.
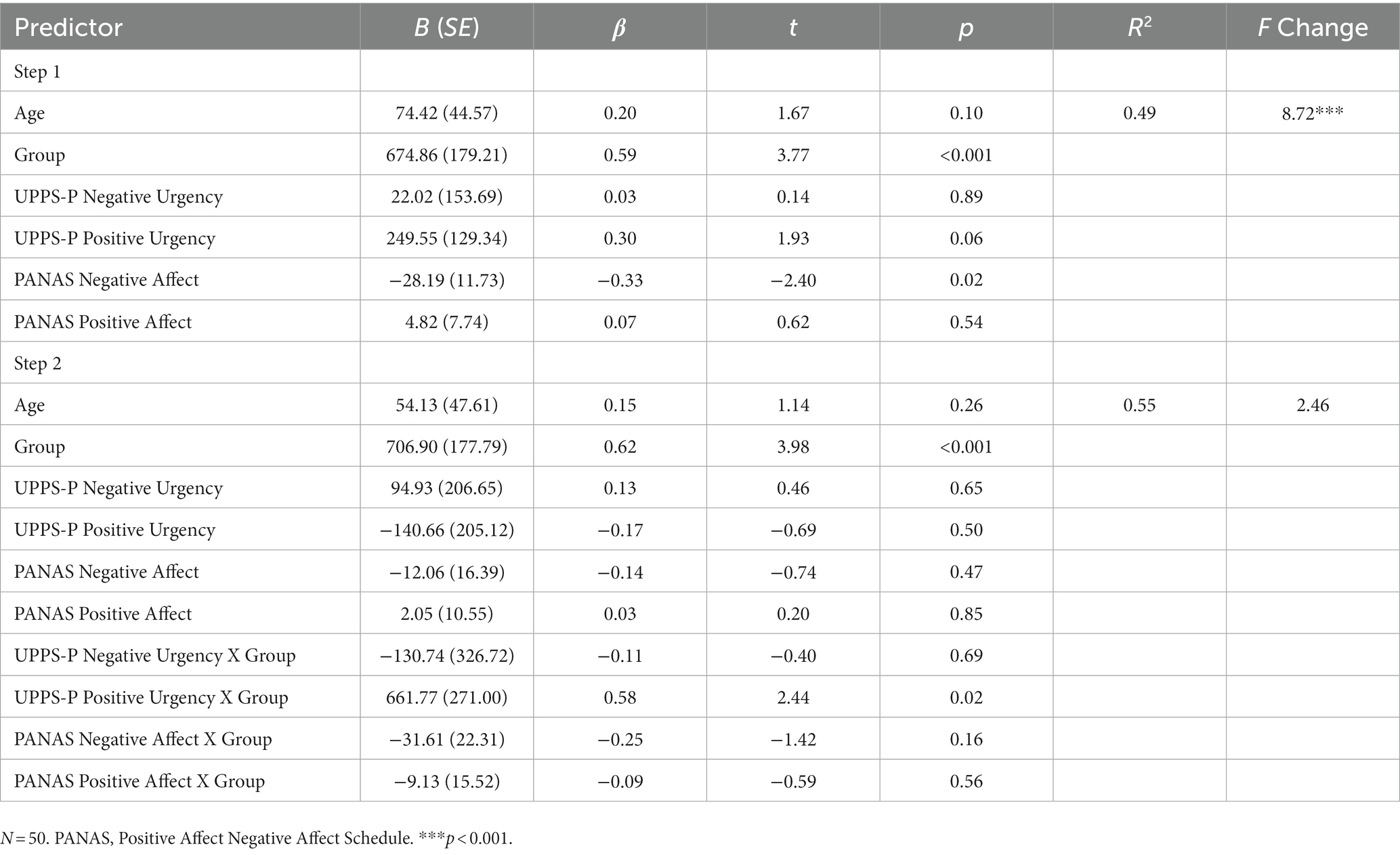
Table 3. Hierarchical linear regression model predicting food consumption in ad lib test meal.
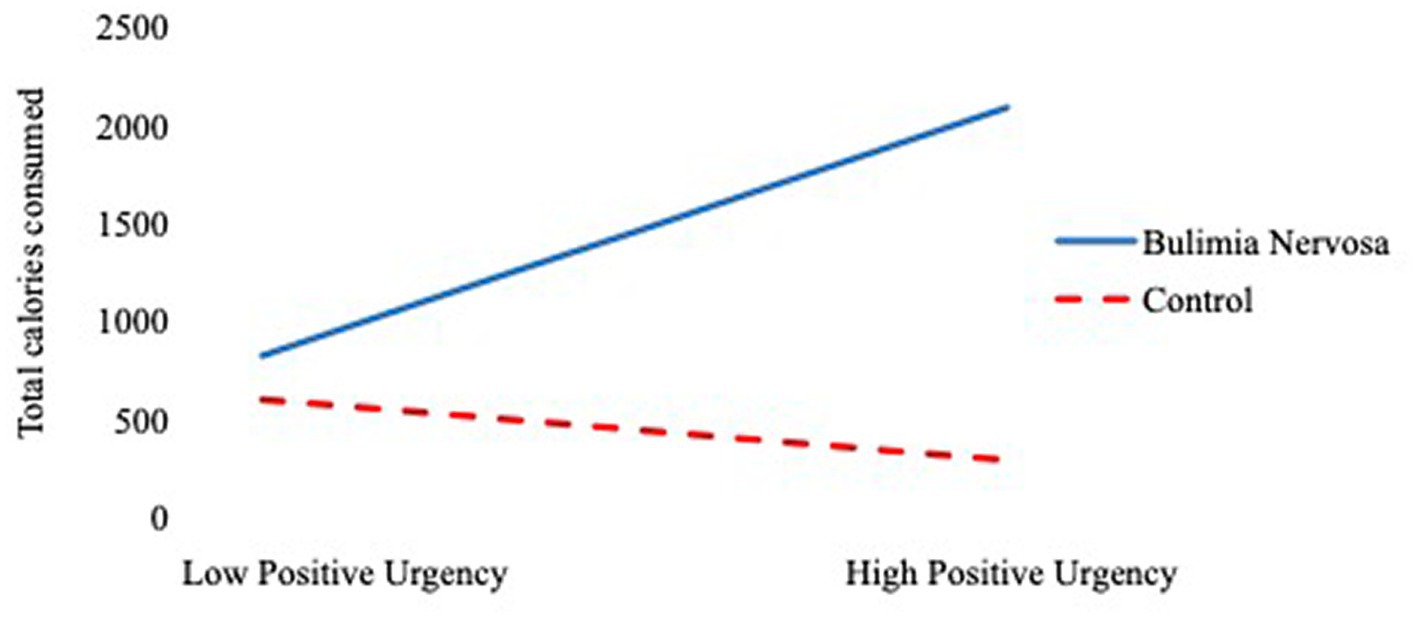
Figure 1. The regression of total calories consumed on positive urgency as a function of group membership.
Discussion
The goal of the current preliminary study was to evaluate dispositional levels of NU and PU in the prediction of binge size among women with BN compared with controls. As expected, women with BN reported higher levels of NU and PU, compared with controls. Hypotheses were partially supported: PU predicted greater ad lib test meal intake among women with BN but not control women. Contrary to our hypothesis, NU was not associated with ad lib test meal intake in women with BN compared to control women. Dispositional levels of broad negative and positive affect also were not significant predictors of test meal intake.
Although prior work has demonstrated cross-sectional associations between PU and self-reported eating disorder symptoms (Claes et al., 2015; Kenny et al., 2019; Michael and Juarascio, 2021), this investigation is the first to support an association between PU and objectively measured binge size among women with BN in a controlled laboratory study. It is striking that PU was the only significant predictor of binge size, above and beyond NU and dispositional levels of negative and positive affect. Results suggest the proneness to act rashly when feeling extreme positive emotions may be uniquely associated with greater binge size in BN. Binge eating episodes frequently include highly palatable foods rated as favorable and rewarding (de Macedo et al., 2016). PU correlates with reward responsiveness (Smith et al., 2023) and predicts other impulsive behaviors perceived as rewarding (e.g., substance use, gambling (Clark et al., 2019; Tanabe et al., 2019)). During the ad lib test meal, we provided participants with BN foods they typically consumed during binge episodes, which were frequently highly palatable (e.g., cookies). It is possible that those with BN and high PU were more likely to find these foods rewarding, and thus more likely to consume a greater amount of food when instructed to binge.
It is surprising that NU did not emerge as a significant predictor of objectively measured binge size in the current study, given associations between BN and NU in prior research (Fischer et al., 2008, 2018). Notably, this result aligns with previous work finding no association between NU and self-reported binge size in BN (Forney et al., 2016). NU may play a central role in the development and maintenance of binge eating behavior (Pearson et al., 2012; Davis and Smith, 2018), but a less prominent role in binge size.
When the interaction of group and PU was not included in the model, higher levels of negative affect were associated with lower caloric intake across participants. Negative affect has been associated with lower calorie intake, which may explain this finding (Moreno-Domínguez et al., 2012). However, it is noteworthy that negative affect was no longer significant when the interaction of group and PU was included in the model. This finding lends support to the notion that it is not just a propensity toward feeling negative or positive emotions that predicts binge size, but perhaps the combination of propensity to experience greater levels of positive affect combined with the tendency to act rashly when experiencing intense emotion.
The literature on binge eating and BN has focused primarily on negative emotion dysregulation. As such, theory regarding positive emotion dysregulation, and, consequently, PU, is underdeveloped (Selby et al., 2019). The current findings indicate PU may be important in the risk process for binge eating. It may be that those with high levels of PU receive positive reinforcement (rather than negative reinforcement) from binge eating. This may be related to elevations in reward sensitivity observed in BN (Harrison et al., 2010). Indeed, women with BN show increased response to eating even when satiated, compared to controls (Bischoff-Grethe et al., 2021), which may contribute to overeating. Increased attention to positive reinforcement would diverge from the historical focus on negative emotion regulation, but may help inform understanding of high PU in BN.
Future studies also may investigate the potential for PU to increase risk for or maintain other forms of eating pathology. Previous work has found PU is also cross-sectionally associated with problematic exercise (Kotbagi et al., 2017). Because PU is associated with impaired decision making (Kräplin et al., 2014) and individuals with binge eating prefer sooner, smaller rewards rather than delayed, larger rewards (Brassard and Balodis, 2021), an individual with BN and high PU may be prompted to binge eat for the short-term positively reinforcing qualities of food intake, but then become worried about the long-term effect of binge eating on their weight. They may then feel prompted, possibly by PU, to engage in behaviors that bring about positive emotions, reduce negative affect about weight gain, and promote weight loss (e.g., exercise; Kotbagi et al., 2017), thus maintaining the binge-compensatory behavior cycle; such a possibility merits investigation. Importantly, this risk process may also extend to other eating disorders, such as anorexia nervosa binge-purge type.
Results suggest assessing PU in BN may be helpful in identifying those at-risk for greater binge size and its consequences. Clinicians should consider a stronger focus on negative and positive emotions during binge eating treatment. Treatments focused on identifying, accepting, and managing negative and positive emotions, such as integrative cognitive-affective therapy, hold promise for reducing BN symptoms (Wonderlich et al., 2014). Interventions emphasizing mindfulness and skills training to regulate emotions, such as dialectical behavior therapy, also have been shown to decrease binge eating (Ben-Porath et al., 2020). Individuals high in PU may benefit from practicing new ways to respond to positive emotions. If one often responds to extreme positive emotions with binge eating, they may instead try calling a loved one or engaging in a sensory activity (e.g., polishing one’s nails). If individuals high in PU experience positive reinforcement from binge eating, they may find it helpful to identify other, more adaptive strategies to elicit positive emotions, such as building mastery in a new hobby.
Interestingly, it is possible that PU may be helpful in facilitating eating disorder recovery; a recent study found that among eating disorder patients, PU was the only personality positively associated with recovery (Cabelguen et al., 2023). Clinicians may find it useful to capitalize on the high levels of positive emotions that accompany PU and potentially promote recovery.
Study strengths included the use of a well-validated laboratory paradigm for binge eating, inclusion of a clinical sample with BN, and use of measures with strong psychometric properties. Limitations are as follows. Our sample consisted of relatively young women. Additionally, group samples were small, although well-powered to detect differences. This study should be replicated in larger samples that are more diverse in terms of gender and age. We used a tightly-controlled laboratory design to test NU and PU’s prediction of binge size, measured objectively. As such, results may or may not reflect binge consumption in one’s everyday life, in their natural environment that is more familiar and less controlled. We cannot know if results would differ if we assessed positive urgency’s prediction of binge size in one’s daily life, as in an ecological momentary assessment design; future research should test that possibility. Finally, given the correlation between PU and NU, replication of the current study to further confirm the role of PU in predicting binge size, using the same controls, is important.
PU appears to be an underappreciated, but potentially important, predictor of binge size in BN. Clinicians and researchers are encouraged to consider PU in their understanding of binge eating in BN.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by University of Kentucky Institutional Review Board. The patients/participants provided their written informed consent to participate in this study.
Author contributions
HD and GS contributed to the conception and design of the study. HD organized the database, performed statistical analyses, and wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This work was supported by a grant from the National Institute of Mental Health (F31 MH114551). The funder had no role in study design, in the data collection, analysis and interpretation of data, in the writing of the report, or in the decision to submit the article for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
APA. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. Virginia: American Psychiatric Association.
Google Scholar
Ben-Porath, D., Duthu, F., Luo, T., Gonidakis, F., Compte, E. J., and Wisniewski, L. (2020). Dialectical behavioral therapy: an update and review of the existing treatment models adapted for adults with eating disorders. Eat. Disord. 28, 101–121. doi: 10.1080/10640266.2020.1723371
PubMed Abstract | CrossRef Full Text | Google Scholar
Berg, J. M., Latzman, R. D., Bliwise, N. G., and Lilienfeld, S. O. (2015). Parsing the heterogeneity of impulsivity: a meta-analytic review of the behavioral implications of the UPPS for psychopathology. Psychol. Assess. 27, 1129–1146. doi: 10.1037/pas0000111
PubMed Abstract | CrossRef Full Text | Google Scholar
Bischoff-Grethe, A., Wierenga, C. E., Bailer, U. F., McClure, S. M., and Kaye, W. H. (2021). Satiety does not alter the ventral striatum’s response to immediate reward in bulimia nervosa. J. Abnorm. Psychol. 130, 862–874. doi: 10.1037/abn0000712
PubMed Abstract | CrossRef Full Text | Google Scholar
Brassard, S. L., and Balodis, I. M. (2021). A review of effort-based decision-making in eating and weight disorders. Prog. Neuro Psychopharmacol. Biol. Psychiatry 110:110333. doi: 10.1016/j.pnpbp.2021.110333
PubMed Abstract | CrossRef Full Text | Google Scholar
Bruzas, M. B., Tronieri, J. S., Chao, A. M., Jones, E., McAllister, C., Gruber, K., et al. (2022). Binge size and loss of control as correlates of eating behavior and psychopathology among individuals with binge eating disorder and higher weight. J. Behav. Med. 45, 603–612. doi: 10.1007/s10865-022-00312-7
PubMed Abstract | CrossRef Full Text | Google Scholar
Cabelguen, C., Saillard, A., Vanier, A., Laslandes, M., Leboucher, J., Rousselet, M., et al. (2023). Is history of abuse predictive of eating disorders with binge-eating episodes through an effect mediated by impulsivity? A French longitudinal study. J. Psychiatry Neurosci. 48, E13–E22. doi: 10.1503/jpn.210218
PubMed Abstract | CrossRef Full Text | Google Scholar
Claes, L., Islam, M. A., Fagundo, A. B., Jimenez-Murcia, S., Granero, R., Agüera, Z., et al. (2015). The relationship between non-suicidal self-injury and the UPPS-P impulsivity facets in eating disorders and healthy controls. PLoS One 10:e0126083. doi: 10.1371/journal.pone.0126083
PubMed Abstract | CrossRef Full Text | Google Scholar
Clark, L., Boileau, I., and Zack, M. (2019). Neuroimaging of reward mechanisms in gambling disorder: an integrative review. Mol. Psychiatry 24, 674–693. doi: 10.1038/s41380-018-0230-2
PubMed Abstract | CrossRef Full Text | Google Scholar
Cooper, Z., and Fairburn, C. (1987). The eating disorder examination: a semi-structured interview for the assessment of the specific psychopathology of eating disorders. Int. J. Eat. Disord. 6, 1–8. doi: 10.1002/1098-108X(198701)6:13.0.CO;2-9
CrossRef Full Text | Google Scholar
Coskunpinar, A., Dir, A. L., and Cyders, M. A. (2013). Multidimensionality in impulsivity and alcohol use: a Meta-analysis using the UPPS model of impulsivity. Alcohol Clin. Exp. Res. 37, 1441–1450. doi: 10.1111/acer.12131
PubMed Abstract | CrossRef Full Text | Google Scholar
Cyders, M. A., and Smith, G. T. (2007). Mood-based rash action and its components: positive and negative urgency. Personal. Individ. Differ. 43, 839–850. doi: 10.1016/j.paid.2007.02.008
CrossRef Full Text | Google Scholar
Davis, H. A., Keel, P. K., Tangney, J. P., and Smith, G. T. (2022). Increases in shame following binge eating among women: Laboratory and longitudinal findings. Appetite, 178:106276.
PubMed Abstract | Google Scholar
de Macedo, I. C., de Freitas, J. S., and da Silva Torres, I. L. (2016). The influence of palatable diets in reward system activation: a Mini review. Adv. Pharmacol. Sci. 2016, 7238679–7238677. doi: 10.1155/2016/7238679
PubMed Abstract | CrossRef Full Text | Google Scholar
DePaoli, L. C., and Sweeney, D. C. (2000). Further validation of the positive and negative affect schedule. J. Soc. Behav. Pers. 15:561.
Google Scholar
Feil, M., Halvorson, M., Lengua, L., and King, K. M. (2020). A state model of negative urgency: do momentary reports of emotional impulsivity reflect global self-report? J. Res. Pers. 86:103942. doi: 10.1016/j.jrp.2020.103942
PubMed Abstract | CrossRef Full Text | Google Scholar
Fischer, S., Smith, G. T., and Cyders, M. A. (2008). Another look at impulsivity: a meta-analytic review comparing specific dispositions to rash action in their relationship to bulimic symptoms. Clin. Psychol. Rev. 28, 1413–1425. doi: 10.1016/j.cpr.2008.09.001
PubMed Abstract | CrossRef Full Text | Google Scholar
Fischer, S., Wonderlich, J., Breithaupt, L., Byrne, C., and Engel, S. (2018). Negative urgency and expectancies increase vulnerability to binge eating in bulimia nervosa. Eat. Disord. 26, 39–51. doi: 10.1080/10640266.2018.1418253
PubMed Abstract | CrossRef Full Text | Google Scholar
Forney, K. J., Bodell, L. P., Haedt-Matt, A. A., and Keel, P. K. (2016). Incremental validity of the episode size criterion in binge-eating definitions: an examination in women with purging syndromes. Int. J. Eat. Disord. 49, 651–662. doi: 10.1002/eat.22508
PubMed Abstract | CrossRef Full Text | Google Scholar
Fox, J. (2019). Regression diagnostics: An introduction. Sage publications.
Google Scholar
Harrison, A., O’Brien, N., Lopez, C., and Treasure, J. (2010). Sensitivity to reward and punishment in eating disorders. Psychiatry Res. 177, 1–11. doi: 10.1016/j.psychres.2009.06.010
CrossRef Full Text | Google Scholar
Johnson, W. G., Schlundt, D. G., Barclay, D. R., Carr-Nangle, R. E., and Engler, L. B. (1995). A naturalistic functional analysis of binge eating. Behav. Ther. 26, 101–118. doi: 10.1016/S0005-7894(05)80085-1
CrossRef Full Text | Google Scholar
Keel, P. K., Bodell, L. P., Forney, K. J., Appelbaum, J., and Williams, D. (2019). Examining weight suppression as a transdiagnostic factor influencing illness trajectory in bulimic eating disorders. Physiol. Behav. 208:112565. doi: 10.1016/j.physbeh.2019.112565
PubMed Abstract | CrossRef Full Text | Google Scholar
Keel, P. K., Haedt-Matt, A. A., Hildebrandt, B., Bodell, L. P., Wolfe, B. E., and Jimerson, D. C. (2018). Satiation deficits and binge eating: probing differences between bulimia nervosa and purging disorder using an ad lib test meal. Appetite 127, 119–125. doi: 10.1016/j.appet.2018.04.009
PubMed Abstract | CrossRef Full Text | Google Scholar
Kenny, T. E., Singleton, C., and Carter, J. C. (2019). An examination of emotion-related facets of impulsivity in binge eating disorder. Eat. Behav. 32, 74–77. doi: 10.1016/j.eatbeh.2018.12.006
PubMed Abstract | CrossRef Full Text | Google Scholar
King, K. M., Feil, M. C., and Halvorson, M. A. (2018). Negative urgency is correlated with the use of reflexive and disengagement emotion regulation strategies. Clin. Psychol. Sci. 6, 822–834. doi: 10.1177/2167702618785619
CrossRef Full Text | Google Scholar
Kissileff, H. R., Wentzlaff, T. H., Guss, J. L., Walsh, B. T., Devlin, M. J., and Thornton, J. C. (1996). A direct measure of satiety disturbance in patients with bulimia nervosa. Physiol. Behav. 60, 1077–1085. doi: 10.1016/0031-9384(96)00086-8
PubMed Abstract | CrossRef Full Text | Google Scholar
Kotbagi, G., Morvan, Y., Romo, L., and Kern, L. (2017). Which dimensions of impulsivity are related to problematic practice of physical exercise? J. Behav. Addict. 6, 221–228. doi: 10.1556/2006.6.2017.024
PubMed Abstract | CrossRef Full Text | Google Scholar
Kräplin, A., Bühringer, G., Oosterlaan, J., Van Den Brink, W., Goschke, T., and Goudriaan, A. E. (2014). Dimensions and disorder specificity of impulsivity in pathological gambling. Addict. Behav. 39, 1646–1651. doi: 10.1016/j.addbeh.2014.05.021
CrossRef Full Text | Google Scholar
Latner, J. D., Hildebrandt, T., Rosewall, J. K., Chisholm, A. M., and Hayashi, K. (2007). Loss of control over eating reflects eating disturbances and general psychopathology. Behav. Res. Ther. 45, 2203–2211. doi: 10.1016/j.brat.2006.12.002
PubMed Abstract | CrossRef Full Text | Google Scholar
Li, N., Mitchison, D., Touyz, S., and Hay, P. (2019). Cross-sectional comparison of health-related quality of life and other features in people with and without objective and subjective binge eating using a general population sample. BMJ Open 9:e024227. doi: 10.1136/bmjopen-2018-024227
PubMed Abstract | CrossRef Full Text | Google Scholar
Lynam, D. R., Smith, G. T., Whiteside, S. P., and Cyders, M. A. (2006). The UPPS-P: Assessing five personality pathways to impulsive behavior In: West Lafayette: Purdue University. 10
PubMed Abstract | Google Scholar
Michael, M. L., and Juarascio, A. (2021). Elevated cognitive dietary restraint mediates the relationship between greater impulsivity and more frequent binge eating in individuals with binge-spectrum eating disorders. Eat. Weight Disord. 26, 2795–2800. doi: 10.1007/s40519-021-01153-0
CrossRef Full Text | Google Scholar
Mitchell, J. E., Crow, S., Peterson, C. B., Wonderlich, S., and Crosby, R. D. (1998). Feeding laboratory studies in patients with eating disorders: a review. Int. J. Eat. Disord. 24, 115–124. doi: 10.1002/(SICI)1098-108X(199809)24:23.0.CO;2-H
CrossRef Full Text | Google Scholar
Moreno-Domínguez, S., Rodríguez-Ruiz, S., Fernández-Santaella, M. C., Ortega-Roldán, B., and Cepeda-Benito, A. (2012). Impact of fasting on food craving, mood and consumption in bulimia nervosa and healthy women participants. Eur. Eat. Disord. Rev. 20, 461–467. doi: 10.1002/erv.2187
PubMed Abstract | CrossRef Full Text | Google Scholar
Mourilhe, C., Moraes, C. E. D., Veiga, G. D., Q da Luz, F., Pompeu, A., Nazar, B. P., et al. (2021). An evaluation of binge eating characteristics in individuals with eating disorders: a systematic review and meta-analysis. Appetite 162:105176. doi: 10.1016/j.appet.2021.105176
PubMed Abstract | CrossRef Full Text | Google Scholar
Pearson, C. M., Combs, J. L., Zapolski, T. C., and Smith, G. T. (2012). A longitudinal transactional risk model for early eating disorder onset. J. Abnorm. Psychol. 121, 707–718. doi: 10.1037/a0027567
PubMed Abstract | CrossRef Full Text | Google Scholar
Pearson, C. M., Wonderlich, S. A., and Smith, G. T. (2015). A risk and maintenance model for bulimia nervosa: from impulsive action to compulsive behavior. Psychol. Rev. 122, 516–535. doi: 10.1037/a0039268
PubMed Abstract | CrossRef Full Text | Google Scholar
Raymond, N. C., Bartholome, L. T., Lee, S. S., Peterson, R. E., and Raatz, S. K. (2007). A comparison of energy intake and food selection during laboratory binge eating episodes in obese women with and without a binge eating disorder diagnosis. Int. J. Eat. Disord. 40, 67–71. doi: 10.1002/eat.20312
PubMed Abstract | CrossRef Full Text | Google Scholar
Safer, D. L. (2015). “Dialectical behavior therapy (DBT) for eating disorders” in Encyclopedia of feeding and eating disorders. ed. T. Wade (Singapore: Springer Singapore), 1–7.
Google Scholar
Schaefer, L. M., Smith, K. E., Anderson, L. M., Cao, L., Crosby, R. D., Engel, S. G., et al. (2020). The role of affect in the maintenance of binge-eating disorder: evidence from an ecological momentary assessment study. J. Abnorm. Psychol. 129, 387–396. doi: 10.1037/abn0000517
PubMed Abstract | CrossRef Full Text | Google Scholar
Selby, E. A., Panza, E., and Plasencia, M. (2019). “Positive emotion dysregulation in eating disorders and obesity” in The Oxford handbook of positive emotion and psychopathology (Oxford: Oxford University Press), 424–443.
Google Scholar
Serafini, K., Malin-Mayor, B., Nich, C., Hunkele, K., and Carroll, K. M. (2016). Psychometric properties of the positive and negative affect schedule (PANAS) in a heterogeneous sample of substance users. Am. J. Drug Alcohol Abuse 42, 203–212. doi: 10.3109/00952990.2015.1133632
PubMed Abstract | CrossRef Full Text | Google Scholar
Smith, G. T., and Cyders, M. A. (2016). Integrating affect and impulsivity: the role of positive and negative urgency in substance use risk. Drug Alcohol Depend. 163, S3–S12. doi: 10.1016/j.drugalcdep.2015.08.038
PubMed Abstract | CrossRef Full Text | Google Scholar
Smith, G. T., Fischer, S., Cyders, M. A., Annus, A. M., Spillane, N. S., and McCarthy, D. M. (2007). On the validity and utility of discriminating among impulsivity-like traits. Assessment 14, 155–170. doi: 10.1177/1073191106295527
PubMed Abstract | CrossRef Full Text | Google Scholar
Smith, K. E., Mason, T. B., Schaefer, L. M., Juarascio, A., Dvorak, R., Weinbach, N., et al. (2020). Examining intra-individual variability in food-related inhibitory control and negative affect as predictors of binge eating using ecological momentary assessment. J. Psychiatr. Res. 120, 137–143. doi: 10.1016/j.jpsychires.2019.10.017
PubMed Abstract | CrossRef Full Text | Google Scholar
Smith, K. E., Wang, W.-L., and Mason, T. B. (2023). (In press). Facets of impulsivity and reward in relation to binge-eating disorder course of illness among children: findings from the adolescent brain cognitive development study. J. Child Psychol. Psychiatry. doi: 10.1111/jcpp.13789 [Epub ahead of print].
CrossRef Full Text | Google Scholar
Sysko, R., Steinglass, J., Schebendach, J., Mayer, L. E. S., and Walsh, B. T. (2018). Rigor and reproducibility via laboratory studies of eating behavior: a focused update and conceptual review. Int. J. Eat. Disord. 51, 608–616. doi: 10.1002/eat.22900
PubMed Abstract | CrossRef Full Text | Google Scholar
Tanabe, J., Regner, M., Sakai, J., Martinez, D., and Gowin, J. (2019). Neuroimaging reward, craving, learning, and cognitive control in substance use disorders: review and implications for treatment. Br. J. Radiol. 92:20180942. doi: 10.1259/bjr.20180942
PubMed Abstract | CrossRef Full Text | Google Scholar
Watson, D., Clark, L. A., and Carey, G. (1988). Positive and negative affectivity and their relation to anxiety and depressive disorders. J. abnorm. psychol. 97, 346.
Google Scholar
Whiteside, S. P., and Lynam, D. R. (2001). The five factor model and impulsivity: using a structural model of personality to understand impulsivity. Personal. Individ. Differ. 30, 669–689. doi: 10.1016/S0191-8869(00)00064-7
CrossRef Full Text | Google Scholar
Wolfe, B., Metzger, E., and Jimerson, D. (2002). Serotonin and satiety in bulimia nervosa. Biol. Psychiatry. 51, 12S–12S.
Google Scholar
Wonderlich, J. A., Breithaupt, L., Thompson, J. C., Crosby, R. D., Engel, S. G., and Fischer, S. (2018). The impact of neural responses to food cues following stress on trajectories of negative and positive affect and binge eating in daily life. J. Psychiatr. Res. 102, 14–22. doi: 10.1016/j.jpsychires.2018.03.005
PubMed Abstract | CrossRef Full Text | Google Scholar
Wonderlich, S. A., Peterson, C. B., Crosby, R. D., Smith, T. L., Klein, M. H., Mitchell, J. E., et al. (2014). A randomized controlled comparison of integrative cognitive-affective therapy (ICAT) and enhanced cognitive-behavioral therapy (CBT-E) for bulimia nervosa. Psychol. Med. 44, 543–553. doi: 10.1017/S0033291713001098
PubMed Abstract | CrossRef Full Text | Google Scholar