Hambleton A, Pepin G, Le A, et al. Psychiatric and medical comorbidities of eating disorders: findings from a rapid review of the literature. J Eat Disord. 2022;10:132.
Google Scholar
Galmiche M, Déchelotte P, Lambert G, et al. Prevalence of eating disorders over the 2000–2018 period: a systematic literature review. Am J Clin Nutr. 2019;109:1402–13.
Google Scholar
Hay P. Current approach to eating disorders: a clinical update. Intern Med J. 2020;50:24–9.
Google Scholar
Karjalainen L, Gillberg C, Råstam M, et al. Eating disorders and eating pathology in young adult and adult patients with ESSENCE. Compr Psychiatr. 2016;66:79–86.
Google Scholar
Qian J, Wu Y, Liu F, et al. An update on the prevalence of eating disorders in the general population: a systematic review and meta-analysis. Eat Weight Disord. 2022;27:415–28.
Google Scholar
American Psychiatric Association, American Psychiatric Association, editors. Feeding and eating disorders. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, D.C: American Psychiatric Association; 2013. pp. 329–54.
Google Scholar
Fichter MM, Quadflieg N, Gnutzmann A. Binge eating disorder: treatment outcome over a 6-year course. J Psychosom Res. 1998;44:385–405.
Google Scholar
Halmi KA. Perplexities of treatment resistence in eating disorders. BMC Psychiatry. 2013;13:292.
Google Scholar
Kim Y-K, editor. Treatment Resistance in Psychiatry: risk factors, Biology, and management. Singapore: Springer Singapore. Epub ahead of print 2019. https://doi.org/10.1007/978-981-10-4358-1
van Hoeken D, Hoek HW. Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Curr Opin Psychiatry. 2020;33:521–7.
Google Scholar
Miskovic-Wheatley J, Bryant E, Ong SH, et al. Eating disorder outcomes: findings from a rapid review of over a decade of research. J Eat Disord. 2023;11:85.
Google Scholar
Keating CT, Hickman L, Leung J et al. Autism-related language preferences of english ‐speaking individuals across the globe: a mixed methods investigation. Autism Research. 2022;aur.2864.
Nickel K, Maier S, Endres D, et al. Systematic review: overlap between eating, autism spectrum, and attention-deficit/hyperactivity disorder. Front Psychiatry. 2019;10:708.
Google Scholar
Villa FM, Crippa A, Rosi E, et al. ADHD and eating disorders in childhood and adolescence: an updated minireview. J Affect Disord. 2023;321:265–71.
Google Scholar
Yao S, Kuja-Halkola R, Martin J, et al. Associations between attention-deficit/hyperactivity disorder and various eating disorders: a Swedish nationwide population study using multiple genetically informative approaches. Biol Psychiatry. 2019;86:577–86.
Google Scholar
Saure E, Laasonen M, Lepistö-Paisley T, et al. Characteristics of autism spectrum disorders are associated with longer duration of anorexia nervosa: a systematic review and meta‐analysis. Int J Eat Disord. 2020;53:1056–79.
Google Scholar
Testa G, Baenas I, Vintró-Alcaraz C, et al. Does ADHD symptomatology influence treatment outcome and dropout risk in eating disorders? A longitudinal study. JCM. 2020;9:2305.
Google Scholar
Zhang R, Birgegård A, Fundín B, et al. Association of autism diagnosis and polygenic scores with eating disorder severity. Euro Eat Disorders Rev. 2022;30:442–58.
Google Scholar
Fernández-Aranda F, Agüera Z, Castro R, et al. ADHD symptomatology in eating disorders: a secondary psychopathological measure of severity? BMC Psychiatry. 2013;13:166.
Google Scholar
Svedlund NE, Norring C, Ginsberg Y, et al. Are attention deficit hyperactivity disorder symptoms stable irrespective of recovery from eating disorders? A 1-year follow‐up of adult females. Eur Eat Disorders Rev. 2021;29:133–43.
Google Scholar
Austin A, Flynn M, Richards K, et al. Duration of untreated eating disorder and relationship to outcomes: a systematic review of the literature. Eur Eat Disorders Rev. 2021;29:329–45.
Google Scholar
Bleck JR, DeBate RD, Olivardia R. The comorbidity of ADHD and eating disorders in a nationally representative sample. J Behav Health Serv Res. 2015;42:437–51.
Google Scholar
Boltri M, Sapuppo W. Anorexia nervosa and autism spectrum disorder: a systematic review. Psychiatry Res. 2021;306:114271.
Google Scholar
Brown CM, Stokes MA. Intersection of eating disorders and the female profile of autism. Child Adolesc Psychiatr Clin N Am. 2020;29:409–17.
Google Scholar
Nazar BP, Bernardes C, Peachey G, et al. The risk of eating disorders comorbid with attention-deficit/hyperactivity disorder: a systematic review and meta-analysis: ADHD comorbid with eating disorders review. Int J Eat Disord. 2016;49:1045–57.
Google Scholar
Numata N, Nakagawa A, Yoshioka K, et al. Associations between autism spectrum disorder and eating disorders with and without self-induced vomiting: an empirical study. J Eat Disord. 2021;9:5.
Google Scholar
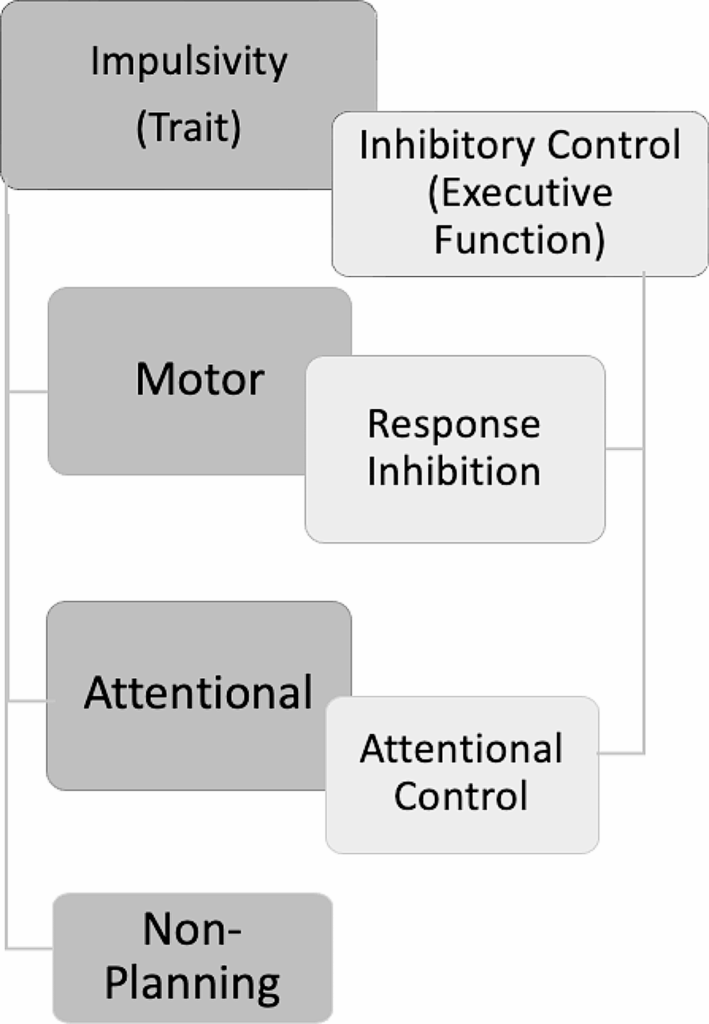
Mirabella G. Inhibitory control and impulsive responses in neurodevelopmental disorders. Dev Med Child Neurol. 2021;63:520–6.
Google Scholar
Pievsky MA, McGrath RE. The neurocognitive profile of attention-deficit/hyperactivity disorder: a review of meta-analyses. Arch Clin Neuropsychol. 2018;33:143–57.
Google Scholar
Reinvall O, Voutilainen A, Kujala T, et al. Neurocognitive functioning in adolescents with autism spectrum disorder. J Autism Dev Disord. 2013;43:1367–79.
Google Scholar
Smith KE, Mason TB, Johnson JS, et al. A systematic review of reviews of neurocognitive functioning in eating disorders: the state-of-the-literature and future directions. Int J Eat Disord. 2018;51:798–821.
Google Scholar
Fithall K, Gray IE, Linardon J, et al. Exploring the role of autistic traits and eating disorder psychopathology on mentalising ability in the general population. BMC Psychol. 2023;11:269.
Google Scholar
Diamond A. Executive functions. Annu Rev Psychol. 2013;64:135–68.
Google Scholar
Dias NM, Helsdingen IE, Lins EKRMD et al. Executive functions beyond the Holy Trinity: a scoping review. Neuropsychology. Epub ahead of print 24 July 2023. https://doi.org/10.1037/neu0000922
Friedman NP, Miyake A. Unity and diversity of executive functions: individual differences as a window on cognitive structure. Cortex. 2017;86:186–204.
Google Scholar
Abramovitch A, Short T, Schweiger A. The C factor: cognitive dysfunction as a transdiagnostic dimension in psychopathology. Clin Psychol Rev. 2021;86:102007.
Google Scholar
Eysenck MW, Moser JS, Derakshan N, et al. A neurocognitive account of attentional control theory: how does trait anxiety affect the brain’s attentional networks? Cogn Emot. 2023;37:220–37.
Google Scholar
Eysenck MW, Derakshan N. New perspectives in attentional control theory. Pers Indiv Differ. 2011;50:955–60.
Google Scholar
Bartholdy S, O’Daly OG, Campbell IC, et al. Neural correlates of failed inhibitory control as an early marker of disordered eating in adolescents. Biol Psychiatry. 2019;85:956–65.
Google Scholar
Eysenck MW, Derakshan N, Santos R, et al. Anxiety and cognitive performance: attentional control theory. Emotion. 2007;7:336–53.
Google Scholar
Zainal NH, Newman MG. Executive functioning constructs in anxiety, obsessive–compulsive, post-traumatic stress, and related disorders. Curr Psychiatry Rep. 2022;24:871–80.
Google Scholar
Bahcivan Saydam R, Ayvasik HB, Alyanak B. Executive functioning in subtypes of attention deficit hyperactivity disorder. Arch Neuropsychiatr. 2015;52:386–92.
Google Scholar
Demetriou EA, DeMayo MM, Guastella AJ. Executive function in autism spectrum disorder: history, theoretical models, empirical findings, and potential as an endophenotype. Front Psychiatry. 2019;10:753.
Google Scholar
Diaz-Marsa M, Pemau A, de la Torre-Luque A, et al. Executive dysfunction in eating disorders: relationship with clinical features. Prog Neuropsychopharmacol Biol Psychiatry. 2023;120:110649.
Google Scholar
Anckarsäter H, Hofvander B, Billstedt E, et al. The sociocommunicative deficit subgroup in anorexia nervosa: autism spectrum disorders and neurocognition in a community-based, longitudinal study. Psychol Med. 2012;42:1957–67.
Google Scholar
Westwood H, Stahl D, Mandy W, et al. The set-shifting profiles of anorexia nervosa and autism spectrum disorder using the Wisconsin card sorting test: a systematic review and meta-analysis. Psychol Med. 2016;46:1809–27.
Google Scholar
Westwood H, Mandy W, Tchanturia K. The association between symptoms of autism and neuropsychological performance in females with anorexia nervosa. Psychiatry Res. 2017;258:531–7.
Google Scholar
Bleck JR. Exploring the underlying mechanisms of comorbid ADHD and eating disorders. ProQuest Inform & Learning, https://ezproxy.deakin.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,sso&db=psyh&AN=2016-21250-232&site=ehost-live&scope=site 2016.
Kaisari P, Dourish CT, Higgs S. Attention deficit hyperactivity disorder (ADHD) and disordered eating behaviour: a systematic review and a framework for future research. Clin Psychol Rev. 2017;53:109–21.
Google Scholar
Seitz J, Kahraman-Lanzerath B, Legenbauer T, et al. The role of impulsivity, inattention and comorbid ADHD in patients with Bulimia Nervosa. PLoS ONE. 2013;8:e63891.
Google Scholar
Faja S, Nelson Darling L. Variation in restricted and repetitive behaviors and interests relates to inhibitory control and shifting in children with autism spectrum disorder. Autism. 2019;23:1262–72.
Google Scholar
Tonizzi I, Giofrè D, Usai MC. Inhibitory control in autism spectrum disorders: meta-analyses on indirect and direct measures. J Autism Dev Disord. Epub ahead of print 23 November 2021. https://doi.org/10.1007/s10803-021-05353-6
Bartholdy S, Rennalls SJ, Jacques C, et al. Proactive and reactive inhibitory control in eating disorders. Psychiatry Res. 2017;255:432–40.
Google Scholar
Wu M, Giel KE, Skunde M, et al. Inhibitory control and decision making under risk in bulimia nervosa and binge-eating disorder: impulsivity in bulimic disorders. Int J Eat Disord. 2013;46:721–8.
Google Scholar
Dalley JW, Everitt BJ, Robbins TW. Impulsivity, compulsivity, and top-down cognitive control. Neuron. 2011;69:680–94.
Google Scholar
Enticott PG, Ogloff JRP, Bradshaw JL. Associations between laboratory measures of executive inhibitory control and self-reported impulsivity. Pers Indiv Differ. 2006;41:285–94.
Google Scholar
Bari A, Robbins TW. Inhibition and impulsivity: behavioral and neural basis of response control. Prog Neurobiol. 2013;108:44–79.
Google Scholar
Gavazzi G, Rossi A, Orsolini S et al. Impulsivity trait and proactive cognitive control: an fMRI study. Eur J Neurosci 2018; ejn.14301.
Leshem R, Yefet M. Does impulsivity converge distinctively with inhibitory control? Disentangling the cold and hot aspects of inhibitory control. Pers Indiv Differ. 2019;145:44–51.
Google Scholar
Weiland BJ, Heitzeg MM, Zald D, et al. Relationship between impulsivity, prefrontal anticipatory activation, and striatal dopamine release during rewarded task performance. Psychiatry Research: Neuroimaging. 2014;223:244–52.
Google Scholar
Coutlee CG, Politzer CS, Hoyle RH et al. An Abbreviated Impulsiveness Scale Constructed Through Confirmatory Factor Analysis of the Barratt Impulsiveness Scale Version 11.
Shen I-H, Lee D-S, Chen C. The role of trait impulsivity in response inhibition: event-related potentials in a stop-signal task. Int J Psychophysiol. 2014;91:80–7.
Google Scholar
Patton H. Factor structure of the barratt impulsiveness scale. Journal of Clinical Psychology; 51.
Nazar BP, Trindade AP, Leslie M, et al. Eating disorders impact on vigilance and decision making of a community sample of treatment naive attention-deficit/hyperactivity disorder young adults. Front Psychiatry. 2018;9:531.
Google Scholar
Rosval L, Steiger H, Bruce K, et al. Impulsivity in women with eating disorders: problem of response inhibition, planning, or attention? Int J Eat Disord. 2006;39:590–3.
Google Scholar
Steadman KM, Knouse LE. Is the relationship between ADHD symptoms and binge eating mediated by impulsivity? J Atten Disord. 2016;20:907–12.
Google Scholar
Claes L, Nederkoorn C, Vandereycken W, et al. Impulsiveness and lack of inhibitory control in eating disorders. Eat Behav. 2006;7:196–203.
Google Scholar
Lijffijt M, Bekker EM, Quik EH, et al. Differences between low and high trait impulsivity are not associated with differences in inhibitory motor control. J Atten Disord. 2004;8:25–32.
Google Scholar
Wilbertz T, Deserno L, Horstmann A, et al. Response inhibition and its relation to multidimensional impulsivity. NeuroImage. 2014;103:241–8.
Google Scholar
Tiego J, Testa R, Bellgrove MA, et al. A hierarchical model of inhibitory control. Front Psychol. 2018;9:1339.
Google Scholar
Banich MT, Depue BE. Recent advances in understanding neural systems that support inhibitory control. Curr Opin Behav Sci. 2015;1:17–22.
Google Scholar
Munakata Y, Herd SA, Chatham CH, et al. A unified framework for inhibitory control. Trends Cogn Sci. 2011;15:453–9.
Google Scholar
Sebastian A, Pohl MF, Klöppel S, et al. Disentangling common and specific neural subprocesses of response inhibition. NeuroImage. 2013;64:601–15.
Google Scholar
Guo N, Fuermaier ABM, Koerts J, et al. Neuropsychological functioning of individuals at clinical evaluation of adult ADHD. J Neural Transm. 2021;128:877–91.
Google Scholar
Collantoni E, Michelon S, Tenconi E, et al. Functional connectivity correlates of response inhibition impairment in anorexia nervosa. Psychiatry Research: Neuroimaging. 2016;247:9–16.
Google Scholar
Kullmann S, Giel KE, Hu X, et al. Impaired inhibitory control in anorexia nervosa elicited by physical activity stimuli. Soc Cogn Affect Neurosci. 2014;9:917–23.
Google Scholar
Fairburn CG. Cognitive behavior therapy and eating disorders. Eating disorders: the transdiagnostic view and the cognitive behavioral theory. Guildford; 2008. http://ebookcentral.proquest.com. accessed 18 May 2020).
Lavender JM, Goodman EL, Culbert KM, et al. Facets of impulsivity and compulsivity in women with anorexia nervosa: impulsivity and compulsivity in AN. Eur Eat Disorders Rev. 2017;25:309–13.
Google Scholar
Stramaccia DF, Penolazzi B, Libardi A, et al. Control over interfering memories in eating disorders. J Clin Exp Neuropsychol. 2018;40:30–44.
Google Scholar
Demeter G, Keresztes A, Harsányi A, et al. Obsessed not to forget: lack of retrieval-induced suppression effect in obsessive-compulsive disorder. Psychiatry Res. 2014;218:153–60.
Google Scholar
Stedal K, Broomfield C, Hay P, et al. Neuropsychological functioning in adult anorexia nervosa: a meta-analysis. Neurosci Biobehavioral Reviews. 2021;130:214–26.
Google Scholar
Mallorquí-Bagué N, Testa G, Lozano‐Madrid M, et al. Emotional and non‐emotional facets of impulsivity in eating disorders: from anorexia nervosa to bulimic spectrum disorders. Eur Eat Disorders Rev. 2020;28:410–22.
Google Scholar
Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73.
Google Scholar
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
Google Scholar
Munn Z, Peters MDJ, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:143.
Google Scholar
Penner I-K, Kobel M, Stöcklin M, et al. The stroop task: comparison between the original paradigm and computerized versions in children and adults. Clin Neuropsychol. 2012;26:1142–53.
Google Scholar
Hong Q, Pluye P, Fàbregues S et al. Mixed Methods Appraisal Tool (MMAT) version 2018. Registration of Copyright (#1148552), 2018.
Kaisari P, Dourish CT, Rotshtein P, et al. Associations between core symptoms of attention deficit hyperactivity disorder and both binge and restrictive eating. Front Psychiatry. 2018;9:103.
Google Scholar
Shaked D, Faulkner LMD, Tolle K, et al. Reliability and validity of the Conners’ continuous performance test. Appl Neuropsychology: Adult. 2020;27:478–87.
Google Scholar
Wöstmann NM, Aichert DS, Costa A, et al. Reliability and plasticity of response inhibition and interference control. Brain Cogn. 2013;81:82–94.
Google Scholar
American Psychiatric Association, American Psychiatric Association, editors. Neurodevelopmental disorders. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, D.C: American Psychiatric Association; 2013. pp. 31–86.
Google Scholar
Schulz K, Fan J, Magidina O, et al. Does the emotional go/no-go task really measure behavioral inhibition? Convergence with measures on a non-emotional analog. Arch Clin Neuropsychol. 2007;22:151–60.
Google Scholar
DeVito EE, Blackwell AD, Clark L, et al. Methylphenidate improves response inhibition but not reflection-impulsivity in children with attention deficit hyperactivity disorder (ADHD). Psychopharmacology. 2009;202:531–9.
Google Scholar
Leshem R. Relationships between trait impulsivity and cognitive control: the effect of attention switching on response inhibition and conflict resolution. Cogn Process. 2016;17:89–103.
Google Scholar
Chmielewski WX, Tiedt A, Bluschke A, et al. Effects of multisensory stimuli on inhibitory control in adolescent ADHD: it is the content of information that matters. NeuroImage: Clin. 2018;19:527–37.
Google Scholar
Polner B, Aichert D, Macare C, et al. Gently restless: association of ADHD-like traits with response inhibition and interference control. Eur Arch Psychiatry Clin Neurosci. 2015;265:689–99.
Google Scholar
Dobson KS, Dozois DJA. Attentional biases in eating disorders: a meta-analytic review of stroop performance. Clin Psychol Rev. 2004;23:1001–22.
Google Scholar
Howard M, Gregertsen EC, Hindocha C, et al. Impulsivity and compulsivity in anorexia and bulimia nervosa: a systematic review. Psychiatry Res. 2020;293:113354.
Google Scholar
Stott N, Fox JRE, Williams MO. Attentional bias in eating disorders: a meta-review. Intl J Eat Disorders. 2021;54:1377–99.
Google Scholar
Svaldi J, Schmitz F, Trentowska M, et al. Cognitive interference and a food-related memory bias in binge eating disorder. Appetite. 2014;72:28–36.
Google Scholar
Martin E, Dourish CT, Hook R, et al. Associations between inattention and impulsivity ADHD symptoms and disordered eating risk in a community sample of young adults. Psychol Med. 2022;52:2622–31.
Google Scholar
Yilmaz Z, Javaras KN, Baker JH, et al. Association between childhood to adolescent attention deficit/hyperactivity disorder symptom trajectories and late adolescent disordered eating. J Adolesc Health. 2017;61:140–6.
Google Scholar
Noebel NA, Oberle CD, Marcell HS. Orthorexia nervosa and executive dysfunction: symptomatology is related to difficulties with behavioral regulation. Eat Weight Disord. Epub ahead of print 8 January 2022. https://doi.org/10.1007/s40519-021-01343-w
Van der Oord S, Braet C, Cortese S, et al. Testing the dual pathway model of ADHD in obesity: a pilot study. Eat Weight Disorders. 2018;23:507–12.
Google Scholar
Hartmann AS, Rief W, Hilbert A. Impulsivity and negative mood in adolescents with loss of control eating and ADHD symptoms: an experimental study. Eat Weight Disorders. 2013;18:53–60.
Google Scholar
Berner LA, Stefan M, Lee S, et al. Altered cortical thickness and attentional deficits in adolescent girls and women with bulimia nervosa. J Psychiatry Neurosci. 2018;43:151–60.
Google Scholar
Cyders MA, Coskunpinar A. Measurement of constructs using self-report and behavioral lab tasks: is there overlap in nomothetic span and construct representation for impulsivity? Clin Psychol Rev. 2011;31:965–82.
Google Scholar
Reynolds B, Ortengren A, Richards JB, et al. Dimensions of impulsive behavior: personality and behavioral measures. Pers Indiv Differ. 2006;40:305–15.
Google Scholar
Stahl C, Voss A, Schmitz F, et al. Behavioral components of impulsivity. J Exp Psychol Gen. 2014;143:850–86.
Google Scholar
Miyake A, Friedman NP. The nature and organization of individual differences in executive functions: four general conclusions. Curr Dir Psychol Sci. 2012;21:8–14.
Google Scholar
Weafer J, Baggott MJ, De Wit H. Test–retest reliability of behavioral measures of impulsive choice, impulsive action, and inattention. Exp Clin Psychopharmacol. 2013;21:475–81.
Google Scholar
Stroop JR. Studies of interference in serial verbal reactions. J Exp Psychol. 1935;18:643–62.
Google Scholar
Friedman NP, Miyake A. The relations among inhibition and interference control functions: a latent-variable analysis. J Exp Psychol Gen. 2004;133:101–35.
Google Scholar
Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16:5–13.
Google Scholar
Christ SE, Holt DD, White DA, et al. Inhibitory control in children with autism spectrum disorder. J Autism Dev Disord. 2007;37:1155–65.
Google Scholar
Valeri G, Casula L, Napoli E, et al. Executive functions and symptom severity in an Italian sample of intellectually able preschoolers with autism spectrum disorder. J Autism Dev Disord. 2020;50:3207–15.
Google Scholar
Lemon JM, Gargaro B, Enticott PG, et al. Brief report: executive functioning in autism spectrum disorders: a gender comparison of response inhibition. J Autism Dev Disord. 2011;41:352–6.
Google Scholar
Yue L, Tang Y, Kang Q, et al. Deficits in response inhibition on varied levels of demand load in anorexia nervosa: an event-related potentials study. Eat Weight Disord. 2020;25:231–40.
Google Scholar
Johansson L, Carlbring P, Ghaderi A, et al. Emotional stroop via internet among individuals with eating disorders: emotional Stroop. Scand J Psychol. 2008;49:69–76.
Google Scholar
Straub ER, Schmidts C, Kunde W, et al. Limitations of cognitive control on emotional distraction – congruency in the color stroop task does not modulate the emotional stroop effect. Cogn Affect Behav Neurosci. 2022;22:21–41.
Google Scholar
Juarascio AS, Manasse SM, Espel HM et al. Could training executive function improve treatment outcomes for eating disorders? Appetite. 2015;90:187–193.
Brockmeyer T, Walther S, Ingenerf K, et al. Brain effects of computer-assisted cognitive remediation therapy in anorexia nervosa: a pilot fMRI study. Psychiatry Research: Neuroimaging. 2016;249:52–6.
Google Scholar
Dandil Y, Baillie C, Tchanturia K. Cognitive remediation therapy as a feasible treatment for a young person with anorexia nervosa and autism spectrum disorder comorbidity: a case study. Clin Case Stud. 2020;19:115–32.
Google Scholar
Dandil Y, Smith K, Adamson J, et al. Individual cognitive remediation therapy benefits for patients with anorexia nervosa and high autistic features. Eur Eat Disorders Rev. 2020;28:87–91.
Google Scholar
Zainal NH, Newman MG. Mindfulness enhances cognitive functioning: a meta-analysis of 111 randomized controlled trials. Health Psychol Rev 2023; 1–27.
Lawler JM, Esposito EA, Doyle CM, et al. A preliminary, randomized-controlled trial of mindfulness and game-based executive function trainings to promote self-regulation in internationally-adopted children. Dev Psychopathol. 2019;31:1513–25.
Google Scholar
Best MW, Gale D, Tran T, et al. Brief executive function training for individuals with severe mental illness: effects on EEG synchronization and executive functioning. Schizophr Res. 2019;203:32–40.
Google Scholar
Manasse SM, Lampe EW, Juarascio AS, et al. Using virtual reality to train inhibitory control and reduce binge eating: a proof-of-concept study. Appetite. 2021;157:104988.
Google Scholar
Haddaway NR, Page MJ, Pritchard CC, et al. PRISMA2020: an R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and open synthesis. Campbell Syst Reviews. 2022;18:e1230.
Google Scholar