1 Introduction
Approximately one million people die annually from diet-related chronic diseases in the United States (U.S.), and these numbers are rising due to prolonged COVID-19 impacts (1). Poor diet is the leading cause of U.S. mortality which is directly related to malnutrition and chronic diseases including type 2 diabetes (T2D), cardiovascular disease (CVD), obesity, and some cancers (2, 3). Almost half of U.S. adults have pre-diabetes (38%) or diabetes (11.3%), with most cases as T2D (4). In 2022, 126.9 million Americans 20 years and older have some form of CVD, comprising approximately 37% of the U.S. population (5). CVD is the leading cause of death for men and women in the U.S., accounting for 695,000 total deaths in 2021 (6). In 2021, diabetes was the eighth leading cause of mortality in the U.S., resulting in 103,294 deaths (7). Diet-related chronic diseases and malnutrition disproportionally affect underserved communities in areas of higher poverty, who do not have access to affordable, healthy, and nutritious foods (8). Access to healthy nutritious foods is an essential social determinant of health (SDOH), and is heavily influenced by local environments and community infrastructure.
The U.S. needs innovative approaches and evidence-based policies to reduce consumption of unhealthy foods and to support accessibility of healthy climate-smart foods and nutritional therapies as part of the “food as medicine” movement. Implementing policies improving American nutrition will significantly impact public health by reducing rates of diet-related chronic diseases, nutrition inequity, and its related healthcare spending. These foods must be widely available, environmentally sustainable, and culturally relevant for vulnerable and impoverished communities.
The current bipartisan 2023–24 U.S. Farm Bill reauthorization presents an opportune time to enact effective and impactful policies to improve America’s nutrition and health. Initially designed in 1933 to address agriculture, the Farm Bill is an omnibus bill which evolved over time to support affordability of healthy foods (9). Significant milestones include the Food Stamp Act of 1964 to provide financial assistance for food security which evolved into the Supplemental Nutrition Assistance Program (SNAP). SNAP is the largest U.S. food assistance program and provides monthly benefits for approximately 40 million low-income Americans, primarily for children, older adults and individuals with disabilities (10). Congress reauthorizes SNAP every 5 years as part of the Farm Bill, which provides policymakers a valuable opportunity to improve healthy nutrition and reduce U.S. diet-related chronic diseases by helping U.S. families gain more access to nutritious foods (11, 12). Effective SNAP implementation must emphasize nutrition equity to reduce diet-related health disparities of low-income Americans (13). For example, lower-income communities consume greater amounts of ultra-processed foods (UPF) resulting in lower quality diets due to their longer shelf life, wide accessibility and lower costs, making them a convenient option for food insecure households and a continuous driver of diet-related chronic disease (14–16). Low income communities are highly targeted by UPF supply chains and are subject to aggressive marketing (16). Consequently, UPF’s are a dominant method of combatting food insecurity, which generates a vicious addiction cycle of maladaptive behavioral preferences as a function of their environmental context (14, 15). Thus, SNAP participants struggle more than higher income groups to meet the U.S. Department of Agriculture (USDA) dietary guidelines and achieve a nutritious diet. Table 1 presents a summary of several SNAP-related programs, the most directly relevant being GusNIP, to support incentivization of fruit and vegetable (F/V) production, distribution, purchasing, and consumption in low-income communities (17).
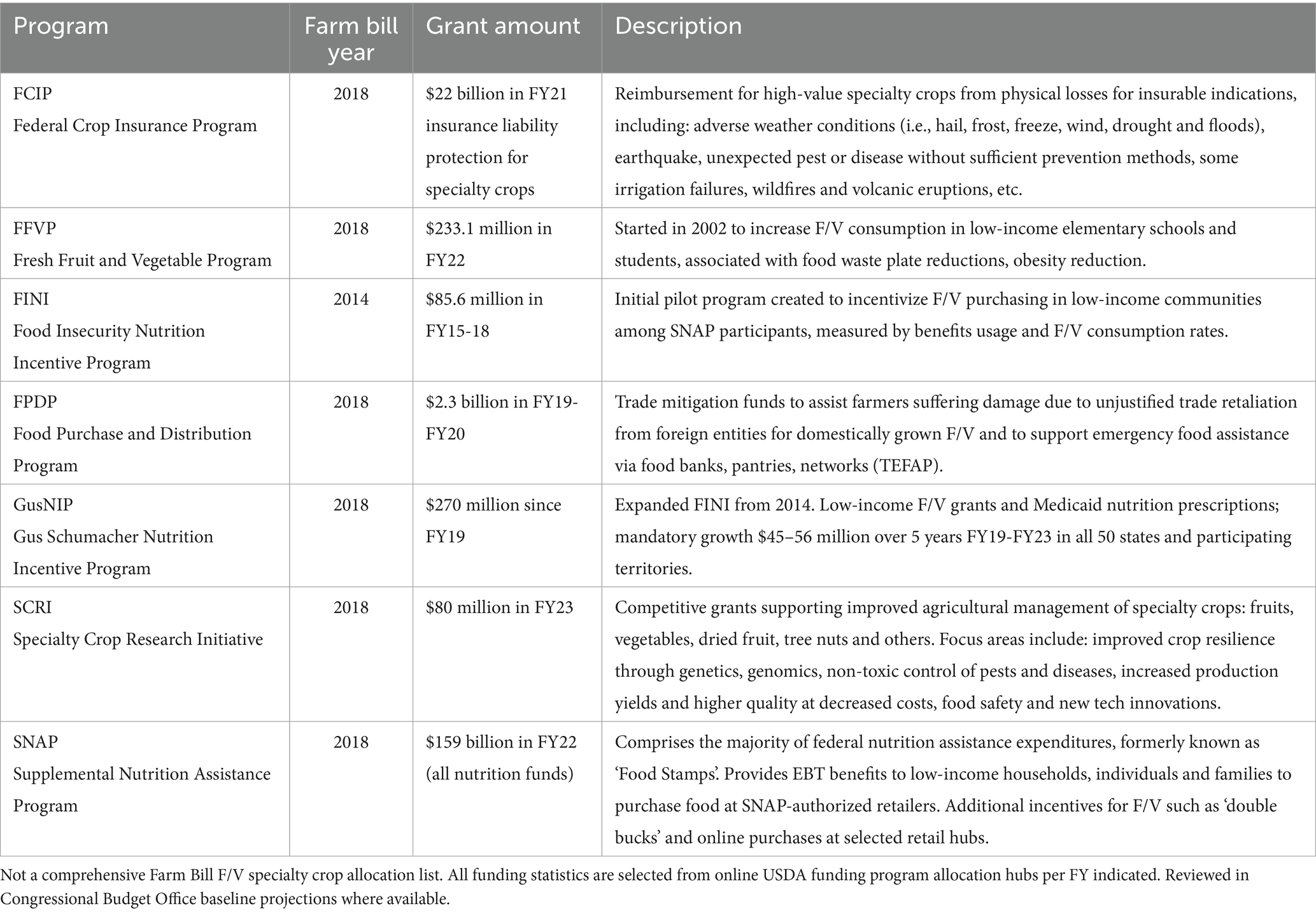
Table 1. Selected key Farm Bill provisions for supporting fruits and vegetables (F/V, specialty crops).
In September 2022, the Biden-Harris administration released the National Strategy on Hunger, Nutrition, and Health, representing the first domestic U.S. policy conference on this topic in over 50 years (18). The federal government’s bipartisan multisector plan to reduce diet-related diseases, improve nutrition, fight hunger and food insecurity, and reduce health disparities comprises five-pillars. Table 2 summarizes each of the five pillars published in the White House’s strategy and highlights selected components relevant to decreasing U.S. diet-related chronic disease (19). The 2023–24 Farm Bill reauthorization provides a valuable post-COVID-19 policy opportunity to improve U.S. health via the participation of a wide variety of strategies, sectors and to strengthen SNAP benefits modalities, coverage and efficacy for low-income Americans (20–22).
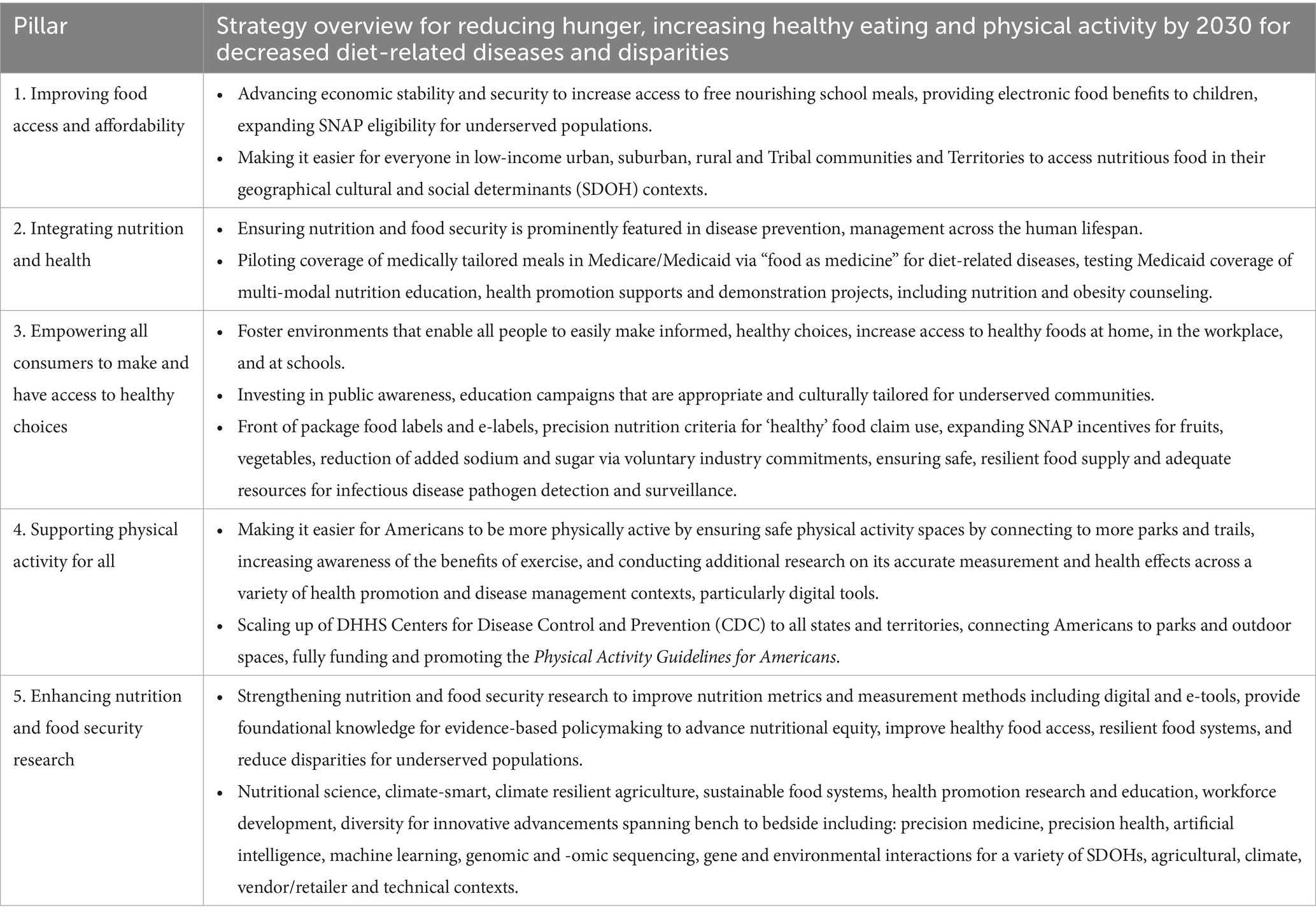
Table 2. Selected components for the 2022 U.S. national strategy to end hunger and build healthy communities.
The goal of this project was to conduct a policy analysis, identify four key strategic food policy insight areas to support equitable U.S. food policy supporting the National Strategy, and formulate options and recommendations for further consideration in this year’s 2023–24 Farm Bill Reauthorization. Our policy analysis question was: what policy options can strengthen U.S. nutrition to promote a healthy, equitable, climate-smart, sustainable food system and reduce diet-related chronic disease?
2 Methods
We performed a policy analysis in Spring 2022 using Centers for Disease Control and Prevention’s (CDC) Policy Analysis Framework tool, depicted in Figure 1 (23). The CDC plays a significant and non-biased role in analyzing policy options for public health problems through the lens of health, economic and budgetary impacts. The Policy Analysis Framework Tool, developed in 2013 by CDC’s Office of Policy, Performance, and Evaluation, aims to strengthen local community through national level policy analysis and strategy planning processes. It does this by appropriately identifying and prioritizing the most impactful public health problems; analyzing and researching policy, health impacts, economic and budgetary gaps to identify possible solutions; developing evidence-based policy intervention options; identifying strategic partnerships that can effect change; aligning key stakeholders for political feasibility; and translating science into practical use implementation and enactment strategies to achieve domestic U.S. health goals.

Figure 1. The CDC policy analytical framework. This project used domains I, II, III of Centers for Disease Control and Prevention (CDC) policy analytical framework process. The CDC policy analysis framework is available in the public domain from the U.S. DHHS (23).
We completed the first three structured domains of the CDC Policy Analysis Framework: problem identification; policy analysis and assess, prioritize available options; and, final policy recommendation for implementation. For problem identification, we conducted a literature review of U.S. food policy topics for focused development, their primary public health impacts, and contributing factors using PubMed, Ovid, CINAHL, Google Scholar, key federal agencies, agency databases and gray literature reports (i.e., Congressional Research Service, U.S. Government Accountability Office, Congressional Budget Office, Centers for Disease Control and Prevention, National Institutes of Health, U.S. Department of Agriculture, etc.). Once the problem and contributory components were identified, additional agency information on key programs, costs, outcome metrics and population statistics were obtained to generate an accurate problem background context and U.S. food policy landscape. Several periods of re-review were conducted (Fall 2022, Spring 2023, Summer 2023) to update evidence, refine selected food policy insight areas, and clarify domestic political landscape issues for which to address U.S. diet-related chronic diseases and nutritional equity. We developed, rated and prioritized policy options based on health, economic and budgetary impacts, political feasibility and analyzed implementation strategy pros/cons across four insight areas: (1) sugar sweetened beverages; (2) food insecurity; (3) reducing UPFs by incentivizing healthy F/V from environmentally sustainable climate-smart agriculture sources; and (4) prioritizing and expanding “food as medicine” nutrition prescriptions. Final policy recommendations and implementation strategies were described in accordance with the evidence.
3 Policy landscape insights and implications
3.1 Policy insight 1 – Sugar sweetened beverages (SSBs)
Sugar-sweetened beverages (SSBs) are considered any liquid with added forms of sugar including regular soda, fruit drinks, sports drinks, energy drinks, sweetened waters, and sweetened coffee and tea drinks (24). According to the 2020–2025 Dietary Guidelines for Americans, added sugars should be limited to less than 10% of daily caloric intake (25). However, SSBs remain inexpensive, widely consumed, are the leading source of modifiable sugar consumption in the U.S. and are linked to increased body mass index and obesity, preventable death/disability, and global diet-related chronic diseases such as T2D and CVD (26–28). U.S. SSB consumption is higher in males, young adults ages 20–39 years, non-Hispanic Black individuals and Mexican Americans, and adults with low incomes below 130% of the poverty line (24, 28). DiFrancesco et al.’s comprehensive trend analysis of sugar intake trends in 72,829 U.S. National Health and Nutrition Examination Survey (NHANES) adult participants from 2001 to 2018, indicated although SSB consumption trends decreased over time, they remained the most significant source of added sugar intake at 37% in 2017–2018 (28). Consumption of artificially sweetened beverages (ASBs) are also associated with developing T2D, CVD, obesity, hypertension and all-cause mortality; however, more scientific evidence is needed to understand conflicting associations, effects strengths and possible carcinogenic impacts at high doses (29).
3.2 Policy insight 2 – Food insecurity
Food secure households maintain consistent food access for a healthy and active lifestyle. In 2022, 12.8% of U.S. households were food insecure, and even reached as high as 20.4% during the lockdown portions of COVID-19 (April 2020), demonstrating increased vulnerability during times of economic disruption and uncertainty (30). Of the 17 million Americans that were food insecure in 2022, they met the thresholds of low (10.2 million) and very low food security (6.8 million) (30). Low food security leads to disruptions in eating patterns and a need for federal assistance such as SNAP benefits, while very low food security results in disrupted patterns and reduced food intake (30). In 2022, 11.7 million adults and 783,000 children, faced very low food security, where food intake steadily decreased throughout the year due to direct lack of money and resources for which to purchase healthy food (30). According to a 2019 national population-based CDC survey, approximately 90% of all Americans do not consume the recommended amounts of F/V (31, 32). Common U.S. barriers to purchasing, preparing and consuming F/V are more pervasive in low resource communities with lower food security and are high priority areas for benefit design prioritization (33). Food insecurity is linked to additional healthcare from skipping and delaying medications and healthcare visits, further perpetuating the problem of poor health (34). U.S. food insecurity demonstrates well-characterized rural and urban geographic, regional patterns with disproportionate impacts on high poverty counties with African American, Alaska Native/American Indian, racial and ethnic minority groups (35, 36). During the COVID-19 pandemic, all U.S. counties were impacted by hunger and food insecurity, and after the pandemic, food insecurity rates among African Americans/Black individuals or Latinos were higher than white individuals in nearly all counties (99%) (36). Nine of ten high food insecurity counties are rural; 82% of the highest food insecurity counties are located in the South and directly linked to unemployment and poverty (35, 36). Current 2024–2034 Congressional Budget Office post-pandemic SNAP projections expect participation of 41.1 million individuals and a 17% cost decrease ($23 billion) due to the end of COVID-19 emergency funds supporting additional food benefits to families with children (37).
3.3 Policy insight 3 – Ultra-processed foods (UPF) and unsustainable food systems
UPFs are foods that have undergone multiple industrial production processes, include frequent use of cosmetic additives for longer shelf-life and hyper-palatability, and involve synthetic formulations of energy dense ingredients including sugar, salt, and trans fats (38). Population based cross-sectional studies indicate UPFs are common staples of the “Westernized diet” for the past two decades (14, 39, 40). They are often found in “food deserts,” where healthful nutrition is minimal, and “food swamps,” where UPF-market retailers dominate the healthier options (41). UPFs induce a high glycemic response, possess low satiety, and account for more than half the total dietary energy consumed in the U.S. (38). Srour et al. (42, 43) found higher UPF grams per day intake was associated with higher risks of CVD, T2D, coronary heart and cerebrovascular disease. “Westernized” UPF eating patterns have grown in prevalence globally and possess both negative human health and environmental impacts (44). Existing obesity, chronic disease and undernutrition health challenges for which UPF contribute, are significantly compounded by climate change, sustainable agriculture and food production availability. Three factors—undernutrition, obesity and climate are a “synergy of pandemics” (45). To reduce UPFs, harmful production and consumption supply chains must be neutralized, while increasing availability of minimally processed nutritious foods sourced from environmentally sustainable agriculture and climate-smart farming practices. Diets lower in animal products generally emit fewer greenhouse gases (GHG) than meat heavy Western diets. Climate smart and resilient foods feature diet diversification with whole grains, legumes, fruits, and vegetables sourced from environmentally sustainable food systems, reduced meat sources, focus on key energy and nutrient crops (i.e., vitamin B12, folate) and parallel agriculture and livestock designs with minimal food waste losses (46, 47). Nutritious dairy, lean meats, and fresh produce grown in protected conditions and/or distributed through air transportation may have higher total GHG environmental impacts despite being very healthy. Ensuring U.S. food and nutrition policy can synergistically advance improvements in both human and environmental health, simultaneously protects both key determinants of human welfare. Per Willet et al. “food is the single strongest lever to optimize human health and environmental sustainability on Earth” (47).
3.4 Policy insight 4 – “Food is medicine” for T2D and CVD
As shown in Table 3, prevalence and financial burdens of T2D, CVD and other diet-related chronic disease has reached epidemic levels; these issues must use a multifactorial approach with diet at the center. “Food is medicine” (or produce prescriptions), is an evidence-based policy approach gaining much interest and favorable feedback from multi-sectoral stakeholders across the political spectrum to facilitate consistent use of USDA-DHHS dietary nutrition guidelines in routine healthcare, especially for those with limited access to healthy foods and health insurance coverage (25, 48). For example, Scrafford et al.’s economic modeling projections estimated $16.7–$31.5 billion healthcare cost savings from conformance with the 2015–2020 U.S. Dietary Guidelines (49). Although protocols vary, several studies indicate U.S. guidelines with greater intakes of whole grains, vegetables, fruits, legumes, nuts and lower intakes of processed foods, meat and poultry, and SSBs, can be tailored to reflect a wide variety of cultural preferences and ethnic traditions (48–50). Community based organizations (CBOs) help ensure appropriateness of “food is medicine” offerings by preserving cultural heritage, while maintaining healthful dietary guidelines and ensuring reduced sugars, saturated fats, and sodium (25, 48–50).
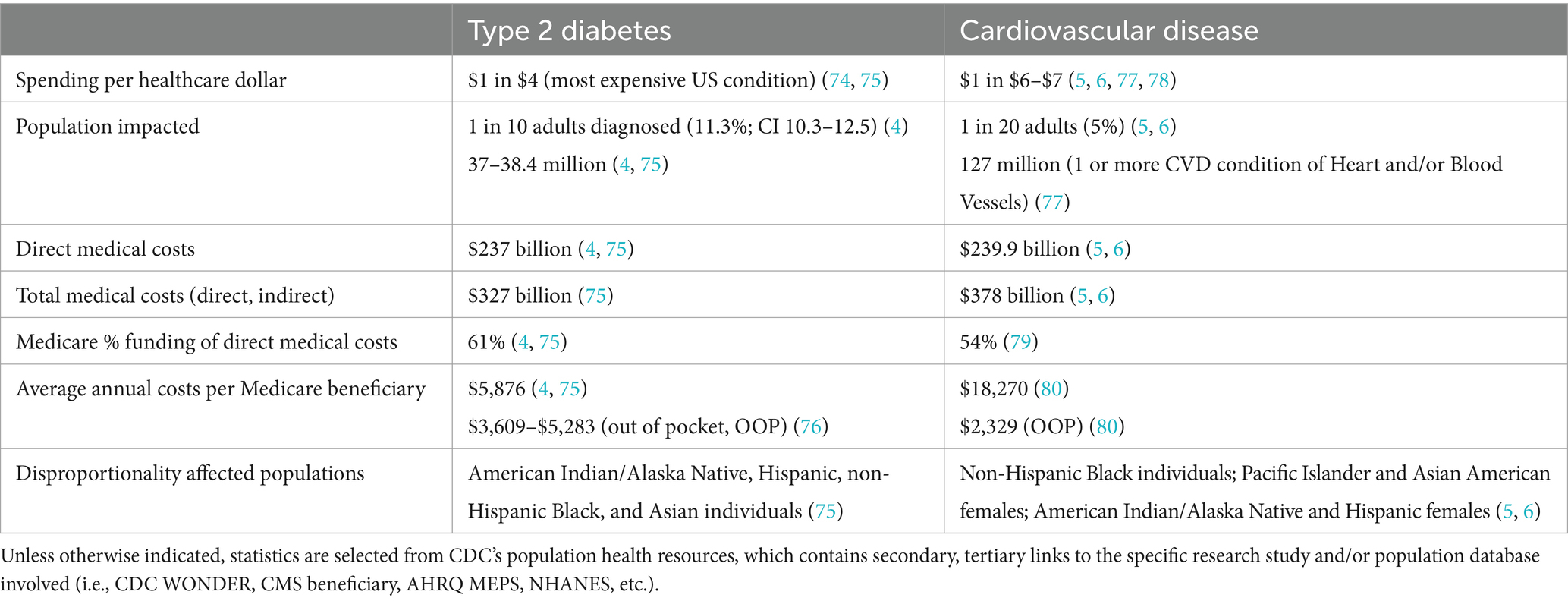
Table 3. U.S. financial burden of diet-related chronic disease.
“Food is medicine” interventions typically feature prescriptions based on a person’s unique health, lifestyle and diet-related disease medical diagnosis requirements that can be linked to insurance reimbursement, care coordination and case management structures. Specific formats include medically tailored meals (MTM), customized groceries, food insecurity produce prescriptions, precision medicine, precision health, and precision nutrition science. Although these disciplines and interventions can help combat diet-related chronic disease and significantly reduce healthcare costs, sufficient scientific evidence is needed for upscaling reimbursable interventions in clinical and community settings, especially for ethnic minority, vulnerable and underserved populations (48, 51–53). For example, Berkowitz et al. found 50% fewer inpatient admissions and 70% fewer emergency department visits for dual eligible Medicare-Medicaid participants that received MTM for 6 months with an average net savings of $220 per patient (54). An additional study by Berkowitz et al. found MTM service with 10 weekly meals was associated with significantly decreased inpatient admissions, fewer skilled nursing facility admissions, and ~ $753 less medical expenditures per person (55). Nutritionally calibrated “food is medicine” interventions, continue to show significant promise by empowering patients and caregivers to optimally prevent and manage chronic diseases and related complications (48).
4 Policy options and final recommendation
Evidence based policy options are summarized next. Table 4 presents the final policy recommendation in addition to detailed implementation advantages, disadvantages.
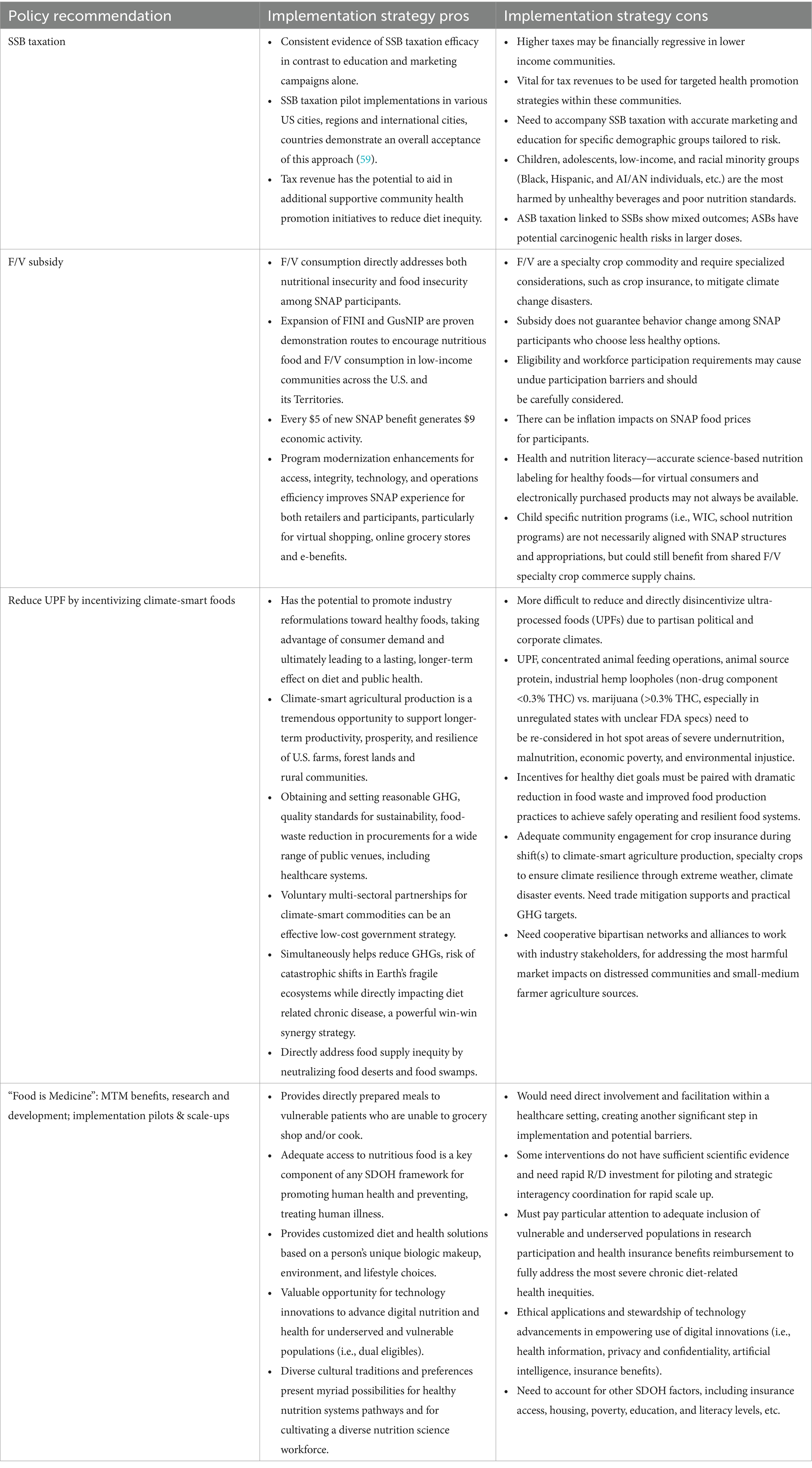
Table 4. Final U.S. food policy recommendation and implementation strategy considerations.
4.1 Policy option 1 – SSB Taxation
Well-designed taxation structures consistently demonstrate evidence of effective SSB consumption decreases contributing to prevention and control of non-communicable diet-related chronic diseases, such that more than 85 countries at national or subnational governance levels use some sort of SSB taxation (56–59). A 20% tax on SSBs, such as that advised by the World Health Organization, can help reduce sugar consumption with little nutritional value by disincentivizing SSB purchases for healthier consumer options, reduce risk of diet-related chronic diseases and strengthen community health (59). For example, Krieger et al. collected data on 7 U.S. cities with a 1–2 cents per ounce SSB excise tax; annual tax revenue was $133.9 million with allocations of $133.2 million back into community infrastructure and programs for a full fiscal year (60). Roberto et al. evaluated a beverage excise tax implemented on both SSBs and ASBs in Philadelphia, resulting in a 51% purchase decrease, but this was offset by increased sales in bordering regions without the tax (61). Price plays a key role in food choice, making SSB tax an important tool to target the largest sugar contributor to the U.S. diet and reduce SSB purchases. Revenue should be allocated into a tax fund with clear specifications, governed for promoting health equity, addressing key SDOH priorities and tailored to community needs.
4.2 Policy option 2 – Healthy food subsidies for F/V
Vendors, retailers and small grocers in high poverty environments have lower access to nutrient dense foods from producers (62). A significant obstacle is that current U.S. F/V subsidy programs are piecemeal and not applied to the entire population. Pomeranz et al. examined the feasibility of various national F/V subsidies in existing local programs and their population health outcome impacts and concluded a nationally mandated subsidy can help reduce diet-related chronic disease and U.S. health economic burdens (62). These programs should be broadly expanded in the 2023–24 Farm Bill and integrated into Electronic Benefits Transfer (EBT) modalities while broadly upscaling other innovative digital program administration and online grocery purchase options that work well for consumer preferences, such as the popular F/V ‘double-bucks’ formats (63–65). Ensuring a greater variety of access, ordering and delivery approaches with online modalities, sufficient Broadband infrastructure and retail hub access will be key to advancing innovative SNAP benefit participation and utilization, especially in rural areas featuring complex interactions between individual state, multi-state, federal and commerce networks (62). Supporting and empowering lower income and underserved communities to strengthen access to healthy, fresh and unprocessed foods at affordable prices, with adequate SNAP benefits, in convenient consumer empowerment formats, even during times of market uncertainty and government crisis (i.e., COVID-19), are key to reducing U.S. nutritional and diet-related health disparities (66, 67).
4.3 Policy option 3 – Incentivize healthy, environmentally sustainable climate-smart foods
Policy options for government regulations reducing consumption of UPFs and food additives, to strengthen promotion of SNAP benefits for minimally processed F/V from sustainably sourced food systems, would greatly improve nutrition, consumer choices supporting specialty growers, products and crops (68, 69). Adherence to mandatory or recommended industry quality standards for limits on unhealthy ingredients and formulations using trans fats, salt, and sugar provide a well-defined approach and yield predictable results based on political feasibility. Although no singular policy on its own can change the U.S. food system to prevent T2D and CVD, thoughtfully designed interconnected policies that mutually reinforce UPF reduction and consumption in vulnerable populations and environmental contexts, are increasingly recognized as a valuable strategy for promoting healthier diets and nutritionally equitable, food secure landscapes (44). Policies to reduce and mitigate UPF harms can be enacted in a step-wise approach, and include front of packages (FOP) warning labels, marketing limitations and ingredient restrictions, particularly for young children, adolescents (44, 70, 71). Several countries have adopted the use of a warning label on UPFs, directly informing consumers leading to a decrease in consumption (44). Since most U.S. rural areas with greater poverty levels rely on mid-size and family farm economies, government must also foster an equitable, climate-smart food system by integrating both human health and environmental sustainability priorities to be sufficiently resilient to withstand natural disasters, adverse weather events and agricultural conditions (72, 73). Climate-smart and sustainable diets should consist largely plant based foods, unsaturated fats, reduced amounts of animal food sources and limited UPFs, trans fats, refined grains, added sugars (45, 47). Government-promoted shifts and bipartisan multi-sectoral collaborations can be harnessed to help ensure the U.S. food system to achieve sustainability, minimize waste byproducts, and stay within necessary boundaries to protect domestic and global earth systems (47, 72). Critical boundaries for consideration include GHG emissions targets, practical feasibility for cropland usage and climate disaster impacts, freshwater usage, nitrogen and phosphorus cycling, and biodiversity loss mitigation.
The EAT-Lancet Commission Report outlines an integrated global framework with quantitative scientific targets for both healthy diets and sustainable food production to avoid severe environmental degradation and prevent approximately 11 million human deaths annually (47). This landmark report recommends regionally tailored healthy diets within optimal caloric intake guidelines comprised of a diversity of plant-based foods and unsaturated fats, while limiting amounts of animal source foods, refined grains, highly processed foods and added sugars to support large scale production and sustainability models.
4.4 Policy option 4 – Incentivize “food is medicine” interventions
Evidence-based “food is medicine” interventions and nutrition access including MTM, medically tailored groceries, precision medicine, nutrition, health and others should be prioritized for research funding and implementation in the U.S. healthcare system (18–20, 52, 53). Risk predictions, pilot interventions and community based supports for Medicare/Medicaid high cost/high need patients (dual-eligibles) and other at-risk populations shouldering high burdens of chronic diet-related illnesses should be especially prioritized if unable to cook or shop for themselves. Patients with high cost chronic conditions T2D, CVD and other diet-related chronic illness should be screened by CBOs within the healthcare SDOH contexts for “food is medicine” intervention eligibility (6, 48, 74). Culturally tailored interventions and community preferences must be honored in clinical and scientific research initiatives. However, Medicare, Medicaid and private insurers should reimburse CBOs, providers, and retailers for “food is medicine” interventions and services to ensure they are available for as many as possible. Healthcare providers should receive reimbursements for screenings according to the strength of evidence from robust federal scientific initiatives, guideline recommendations and population level nutritional surveillance programs.
5 Conclusion
U.S. nutrition and diet-related chronic diseases are at epidemic levels, were greatly exacerbated by COVID-19, and continue to extensively evolve to accommodate consumer preferences and food system supply/demand workflows. UPFs and SSBs are a core part of the U.S. food system continuing to drive chronic disease prevalence and severity, while disproportionally impacting lower income households. The U.S. must begin to impactfully address the abundance of these extremely unhealthy food products while better supporting the food systems capable of producing minimally processed, environmentally sustainable and nutrient rich F/V sources for dietary health guideline compliance. U.S. food policy must be tailored to address key SDOH driving health disparities. The lack of nutritious and affordable foods in lower income areas are due to supply chain inadequacies manifesting as food deserts and food swamps overridden with cheap UPFs. U.S. food policy also must account for rapidly altered post-COVID-19 digital landscapes, technological healthcare and commercial agriculture advances, in order to foster food industry and benefits management innovations that ensure no one is left behind. Learning from COVID-19’s food supply chain lessons, the 2023–24 Farm Bill renewal presents a valuable time to implement robust and impactful U.S. SNAP benefit modernization to reduce the rates of diet-related chronic disease health disparities, support low-income communities, strengthen access to sustainable, resilient, climate friendly food systems, and implement “food is medicine” approaches.
Using a reputable national policy analysis framework tool, this policy brief provides cutting edge, evidence-based policy solutions, in direct consideration for the 2023–24 Farm Bill Reauthorization. Our findings and recommendations are aligned with the bipartisan 2022 White House Council on Hunger Health and Nutrition, the first conference on this topic in over 50 years. Policy recommendations are not just based in scientific evidence, but are also in direct alignment with the political feasibility and stated preferences of a number of bipartisan stakeholders. The crucial issues identified by this food policy analysis project support a number of key strategic priority areas for advancing U.S. human health and nutrition including: achieving racial and nutritional equity, reducing healthcare costs for diet-related chronic diseases, supporting post-COVID-19 recovery and supply chain innovation and growth, and promoting climate-smart agriculture for specialty crops.
Author contributions
EM: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. EK-T: Conceptualization, Course design, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
In Spring 2022, EK-T served as lead faculty in the syllabus design and instruction of NURS-624 (Foundations of Health Systems and Health Policy), a core course in the Clinical Nurse Leader Program. We are grateful to Georgetown Institute for Women, Peace and Security for supporting this project and providing an institutional affiliation for authorized use of Georgetown University’s library services. Grateful acknowledgement is also extended to the White House (WH) Conference on Hunger, Nutrition and Health (7/2022-present) and WH Rural Partners Network Updates (7/2023-present).
Conflict of interest
EM is currently employed by Holy Cross Hospital as a Staff Nurse in the Emergency Room. EK-T was employed by Georgetown University as an Adjunct Associate Professor in a contract capacity for the School of Nursing and Health Studies in Spring 2022-Fall 2022, and School of Nursing in Spring 2023. EK-T is currently an unpaid volunteer guest researcher with the role title ‘Sponsored University Associate’ at the Georgetown Institute for Women, Peace and Security (GIWPS), affiliated with the Walsh School of Foreign Service. EK-T is self-employed by Precision Policy Solutions, LLC.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. U.S. Burden of Disease Collaborators. The state of US health, 1990-2016: burden of diseases, injuries, and risk factors among US states. JAMA. (2018) 319:1444–72. doi: 10.1001/jama.2018.0158
PubMed Abstract | Crossref Full Text | Google Scholar
5. Tsao, CW, Aday, AW, Almarzooq, ZI, Alonso, A, Beaton, AZ, Bittencourt, MS, et al. Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation. (2022) 145:e153–639. doi: 10.1161/CIR.0000000000001052
PubMed Abstract | Crossref Full Text | Google Scholar
13. Fang Zhang, F, Liu, J, Rehm, CD, Wilde, P, Mande, JR, and Mozaffarian, D. Trends and disparities in diet quality among US adults by supplemental nutrition assistance program participation status. JAMA Netw Open. (2018) 1:e180237. doi: 10.1001/jamanetworkopen.2018.0237
PubMed Abstract | Crossref Full Text | Google Scholar
14. Lane, M, Davis, J, Beattie, S, Gomez-Donoso, C, Loughman, A, O’Neil, A, et al. Ultraprocessed food and chronic noncommunicable diseases: a systematic review and meta-analysis of 43 observational studies. Obes Rev. (2020) 22:e13146. doi: 10.1111/obr.13146
PubMed Abstract | Crossref Full Text | Google Scholar
15. Rehm, CD, Monsivais, P, and Drewnowski, A. Relation between diet cost and healthy eating index 2010 scores among adults in the United States 2007-2010. Prev Med. (2015) 73:70–5. doi: 10.1016/j.ypmed.2015.01.019
PubMed Abstract | Crossref Full Text | Google Scholar
16. Leung, CW, Fulay, AP, Parnarouskis, L, Martinez-Steele, E, Gearhardt, AN, and Wolfson, JA. Food insecurity and ultra-processed food consumption: the modifying role of participation in the supplemental nutrition assistance program (SNAP). Am J Clin Nutr. (2022) 116:197–205. doi: 10.1093/ajcn/nqac049
PubMed Abstract | Crossref Full Text | Google Scholar
26. Alcaraz, A, Pichon-Riviere, A, Palacios, A, Bardach, A, Balan, D, Perelli, L, et al. Sugar sweetened beverages attributable disease burden and the potential impact of policy interventions: a systematic review of epidemiological and decision models. BMC Public Health. (2021) 21:1460. doi: 10.1186/s12889-021-11046-7
PubMed Abstract | Crossref Full Text | Google Scholar
28. DiFrancesco, L, Fulgoni, VL, Gaine, PC, Scott, MO, and Ricciuto, L. Trends in added sugars intake and sources among U.S. adults using the National Health and nutrition examination survey (NHANES) 2001-2018. Front Nutr. (2022) 9:897952. doi: 10.3389/fnut.2022.897952
Crossref Full Text | Google Scholar
29. Diaz, C, Rezende, LFM, Sabag, A, Lee, DH, Ferrari, G, Giovannucci, EL, et al. Artificially sweetened beverages and health outcomes: an umbrella review. Adv Nutr. (2023) 14:710–7. doi: 10.1016/j.advnut.2023.05.010
PubMed Abstract | Crossref Full Text | Google Scholar
31. Lee, SH, Moore, LV, Park, S, Harris, DM, and Blanck, HM. Adults meeting fruit and vegetable intake recommendations – United States, 2019. Morb Mortal Wkly Rep. (2022) 71:1–9. doi: 10.15585/mmwr.mm7101a1
PubMed Abstract | Crossref Full Text | Google Scholar
32. Kim-Mozeleski, JE, Pike Moore, SN, Trapl, ES, Perzynski, AT, Tsoh, JY, and Gunzler, DD. Food insecurity trajectories in the US during the first year of the COVID-19 pandemic. Prev Chronic Dis. (2023) 20:E03. doi: 10.5888/pcd20.220212
PubMed Abstract | Crossref Full Text | Google Scholar
33. Wiese, GN, Ramakrishnan, M, Clark, C, and Savaiano, D. Incentivizing fruits and vegetables in the farm bill. Nutr Today. (2020) 55:168–73. doi: 10.1097/NT.0000000000000423
Crossref Full Text | Google Scholar
34. Berkowitz, SA, Basu, S, Gundersen, C, and Seligman, HK. State-level and county-level estimates of health care costs associated with food insecurity. Prev Chronic Dis. (2019) 16:E90. doi: 10.5888/pcd16.180549
PubMed Abstract | Crossref Full Text | Google Scholar
35. Gundersen, C, Dewey, A, Crumbaugh, A, Kato, M, Engelhard, E, Odeen, B, et al. Map the meal gap 2018: an analysis of county and congressional district food insecurity and county food cost in the United States in 2016. Chicago, IL: Feeding America (2018). Available at: https://www.feedingamerica.org/sites/default/files/research/map-the-meal-gap/2016/2016-map-the-meal-gap-full.pdf.
Google Scholar
38. Monteiro, CA, Cannon, G, Levy, RB, Moubarac, JC, Louzada, ML, Rauber, F, et al. Ultra-processed foods: what they are and how to identify them. Public Health Nutr. (2019) 22:936–41. doi: 10.1017/S1368980018003762
PubMed Abstract | Crossref Full Text | Google Scholar
40. Juul, F, Parekh, N, Martinez-Steele, E, Monteiro, C, and Chang, V. Ultra-processed food consumption among U.S. adults from 2001-2018. Am J Clin Nutr. (2022) 115:211–21. doi: 10.1093/ajcn/nqab305
PubMed Abstract | Crossref Full Text | Google Scholar
41. Cooksey Stowers, K, Jiang, Q, Atoloye, A, Lucan, S, and Gans, K. Racial differences in perceived food swamp and food desert exposure and disparities in self-reported dietary habits. Int J Environ Res Public Health. (2020) 17:7143. doi: 10.3390/ijerph17197143
PubMed Abstract | Crossref Full Text | Google Scholar
42. Srour, B, Fezeu, LK, Kesse-Guyot, E, Allès, B, Méjean, C, Andrianasolo, RM, et al. Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé). BMJ. (2019) 365:l1451. doi: 10.1136/bmj.l1451
PubMed Abstract | Crossref Full Text | Google Scholar
43. Srour, B, Fezeu, LK, Kesse-Guyot, E, Allès, B, Debras, C, Druesne-Pecollo, N, et al. Ultraprocessed food consumption and risk of type 2 diabetes among participants of the NutriNet-Santé prospective cohort. JAMA Intern Med. (2020) 180:283–91. doi: 10.1001/jamainternmed.2019.5942
PubMed Abstract | Crossref Full Text | Google Scholar
44. Popkin, B, Barquera, S, Corvalan, C, Hofman, K, Monteiro, C, Ng, S, et al. Toward unified and impactful policies for reducing ultraprocessed food consumption and promoting healthier eating globally. Lancet Diabetes Endocrinol. (2021) 9:462–70. doi: 10.1016/S2213-8587(21)00078-4
PubMed Abstract | Crossref Full Text | Google Scholar
45. Swinburn, BA, Kraak, VI, Allender, S, Atkins, VJ, Baker, PI, Bogard, JR, et al. The global syndemic of obesity, undernutrition, and climate change: the lancet commission report. Lancet. (2019) 393:791–846. doi: 10.1016/S0140-6736(18)32822-8
PubMed Abstract | Crossref Full Text | Google Scholar
46. Geyik, O, Hadjikakou, M, and Bryan, B. Climate-friendly and nutrition-sensitive interventions can close the global dietary nutrient gap while reducing GHG emissions. Nature Food. (2023) 4:61–73. doi: 10.1038/s43016-022-00648-y
PubMed Abstract | Crossref Full Text | Google Scholar
47. Willett, W, Rockström, J, Loken, B, Springmann, M, Lang, T, Vermeulen, S, et al. Food in the anthropocene: the EAT-lancet commission on healthy diets from sustainable food systems. Lancet. (2019) 393:447–92. doi: 10.1016/S0140-6736(18)31788-4
PubMed Abstract | Crossref Full Text | Google Scholar
48. Downer, S, Berkowitz, SA, Harlan, TS, Olstad, DL, and Mozaffarian, D. Food is medicine: actions to integrate food and nutrition into healthcare. BMJ. (2020) 369:m2482. doi: 10.1136/bmj.m2482
PubMed Abstract | Crossref Full Text | Google Scholar
49. Scrafford, CG, Bi, X, Multani, JK, Murphy, MM, Schmier, JK, and Barraj, LM. Health economic evaluation modeling shows potential health care cost savings with increased conformance with healthy dietary patterns among adults in the United States. J Acad Nutr Diet. (2019) 119:599–616. doi: 10.1016/j.jand.2018.10.002
PubMed Abstract | Crossref Full Text | Google Scholar
50. Shan, Z, Li, Y, Baden, Y, Bhuoathiraju, S, Wang, D, Sun, Q, et al. Association between healthy eating patterns and risk of cardiovascular disease. JAMA Intern Med. (2020) 180:1090–100. doi: 10.1001/jamainternmed.2020.2176
PubMed Abstract | Crossref Full Text | Google Scholar
51. Hager, K, Cudhea, FP, Wong, JB, Berkowitz, SA, Downer, S, Lauren, BN, et al. Association of national expansion of insurance coverage of medically tailored meals with estimated hospitalizations and health care expenditures in the US. JAMA Netw Open. (2022) 5:e2236898. doi: 10.1001/jamanetworkopen.2022.36898
PubMed Abstract | Crossref Full Text | Google Scholar
52. Fu, MR, Kurnat-Thoma, E, Starkweather, A, Henderson, WA, Cashion, AK, Williams, JK, et al. Precision health: a nursing perspective. Int J Nurs Sci. (2019) 7:5–12. doi: 10.1016/j.ijnss.2019.12.008
PubMed Abstract | Crossref Full Text | Google Scholar
53. National Academies of Sciences, Engineering, and Medicine. Challenges and opportunities for precision and personalized nutrition: proceedings of a workshop. Washington, DC: The National Academies Press (2022). doi:10.17226/26299
Crossref Full Text | Google Scholar
54. Berkowitz, SA, Terranova, J, Hill, C, Ajayi, T, Linsky, T, Tishler, LW, et al. Meal delivery programs reduce the use of costly health care in dually eligible Medicare and Medicaid beneficiaries. Health Aff. (2018) 37:535–42. doi: 10.1377/hlthaff.2017.0999
PubMed Abstract | Crossref Full Text | Google Scholar
55. Berkowitz, SA, Terranova, J, Randall, L, Cranston, K, Waters, DB, and Hsu, J. Association between receipt of a medically tailored meal program and health care use. JAMA Intern Med. (2019) 179:786–93. doi: 10.1001/jamainternmed.2019.0198
PubMed Abstract | Crossref Full Text | Google Scholar
56. Andreyeva, T, Marple, K, Marinello, S, Moore, TE, and Powell, LM. Outcomes following taxation of sugar-sweetened beverages: a systematic review and meta-analysis. JAMA Netw Open. (2022) 5:e2215276. doi: 10.1001/jamanetworkopen.2022.15276
PubMed Abstract | Crossref Full Text | Google Scholar
57. Pfinder, M, Heise, TL, Hilton Boon, M, Pega, F, Fenton, C, Griebler, U, et al. Taxation of unprocessed sugar or sugar-added foods for reducing their consumption and preventing obesity or other adverse health outcomes. Cochrane Database Syst Rev. (2020) 2020:CD012333. doi: 10.1002/14651858.CD012333.pub2
PubMed Abstract | Crossref Full Text | Google Scholar
58. Hajishafiee, M, Kapellas, K, Listl, S, Pattamatta, M, Gkekas, A, and Moynihan, P. Effect of sugar-sweetened beverage taxation on sugars intake and dental caries: an umbrella review of a global perspective. BMC Pub Heal. (2023) 23:986. doi: 10.1186/s12889-023-15884-5
PubMed Abstract | Crossref Full Text | Google Scholar
60. Krieger, J, Magee, K, Hennings, T, Schoof, J, and Madsen, KA. How sugar-sweetened beverage tax revenues are being used in the United States. Prev Med Rep. (2021) 23:101388. doi: 10.1016/j.pmedr.2021.101388
PubMed Abstract | Crossref Full Text | Google Scholar
61. Roberto, CA, Lawman, HG, LeVasseur, MT, Mitra, N, Peterhans, A, Herring, B, et al. Association of a beverage tax on sugar-sweetened and artificially sweetened beverages with changes in beverage prices and sales at chain retailers in a large urban setting. JAMA. (2019) 321:1799–810. doi: 10.1001/jama.2019.4249
PubMed Abstract | Crossref Full Text | Google Scholar
62. Pomeranz, JL, Huang, Y, Mozaffarian, D, and Micha, R. Legal feasibility and implementation of federal strategies for a national retail-based fruit and vegetable subsidy program in the United States. Milbank Q. (2020) 98:775–801. doi: 10.1111/1468-0009.12461
PubMed Abstract | Crossref Full Text | Google Scholar
63. Durward, C, Savoie-Roskos, M, Atoloye, A, Isabella, P, Jewkes, M, Ralls, B, et al. Double up food bucks participation is associated with increased F/V consumption and food security among low-income adults. J Nutr Educ Behav. (2018) 51:342–7. doi: 10.1016/j.jneb.2018.08.011
PubMed Abstract | Crossref Full Text | Google Scholar
64. Cohen, A, Oatmen, K, Heisler, M, Hesterman, O, Murphy, E, Zick, S, et al. Facilitators and barriers to SNAP incentive use: findings from a clinic intervention for low-income patients. Am J Prev Med. (2019) 56:571–9. doi: 10.1016/j.amepre.2018.11.010
PubMed Abstract | Crossref Full Text | Google Scholar
65. Parks, C, Han, P, Fricke, H, Parker, H, Hesterman, O, and Yaroch, A. Reducing food insecurity and improving F/V intake through a nutrition incentive program in Michigan, USA. SSM Popul Health. (2021) 15:100898. doi: 10.1016/j.ssmph.2021.100898
PubMed Abstract | Crossref Full Text | Google Scholar
66. Rummo, PE, Roberto, CA, Thorpe, LE, Troxel, AB, and Elbel, B. Effect of financial incentives and default options on food choices of adults with low income in online retail settings: a randomized clinical trial. JAMA Netw Open. (2023) 6:e232371. doi: 10.1001/jamanetworkopen.2023.2371
PubMed Abstract | Crossref Full Text | Google Scholar
67. Consavage Stanley, K, Harrigan, PB, Serrano, EL, and Kraak, VI. Applying a multi-dimensional digital food and nutrition literacy model to inform research and policies to enable adults in the U.S. supplemental nutrition assistance program to make healthy purchases in the online food retail ecosystem. Int J Environ Res Public Health. (2021) 18:8335. doi: 10.3390/ijerph18168335
PubMed Abstract | Crossref Full Text | Google Scholar
68. Bleich, SN, Sullivan, K, Broad Leib, E, Dunn, CG, Woteki, C, Yaroch, AL, et al. Strengthening the public health impacts of SNAP: Key opportunities for the next farm bill. Robert Wood Johnson Foundation. Durham, NC: Healthy Eating Research (2021). Available at: https://healthyeatingresearch.org/wordpress/wp-content/uploads/2021/05/her-snap-farm-bill-executive-summary-pdf.
Google Scholar
69. Dulin-Keita, A, Quintilliani, LM, Buscemi, J, Bell, BM, Gans, KM, and Yaroch, AL. Society of behavioral medicine position statement: increase funding for fruits and vegetables production in the farm bill reauthorization. Transl Behav Med. (2019) 9:391–4. doi: 10.1093/tbm/iby041
PubMed Abstract | Crossref Full Text | Google Scholar
70. Taillie, LS, Hall, MG, Popkin, BM, Ng, SW, and Murukutla, N. Experimental studies of front-of-package nutrient warning labels on sugar-sweetened beverages and ultra-processed foods: a scoping review. Nutrients. (2020) 12:569. doi: 10.3390/nu12020569
PubMed Abstract | Crossref Full Text | Google Scholar
71. Song, J, Brown, M, Tan, M, MacGregor, G, Webster, J, Campbell, N, et al. Impact of color-coded and warning nutrition labelling schemes: a systematic review and network meta-analysis. PLoS Med. (2021) 18:e1003765. doi: 10.1371/journal.pmed.1003765
PubMed Abstract | Crossref Full Text | Google Scholar
72. Klytchnikova, I, Sadler, M, Townsend, R, Edmeades, S, Choudhary, V, Hussain, S, et al. Future of food: shaping a climate-smart global food system (English). Washington, DC: World Bank Group (2015). Available at: https://documents.worldbank.org/en/publication/documents-reports/documentdetail/645981468189237140/future-of-food-shaping-a-climate-smart-global-food-system.
Google Scholar
76. Park, J, Zhang, P, Wang, Y, Zhou, X, Look, K, and Bigman, E. High out-of-pocket (OOP) health care cost burden among Medicare beneficiaries with diabetes, 1999-2017. Diabetes Care. (2021) 44:1797–804. doi: 10.2337/dc20-2708
PubMed Abstract | Crossref Full Text | Google Scholar
77. Coronado, F, Melvin, S, Bell, R, and Zhao, G. Preventing chronic disease. Global responses to prevent manage and control cardiovascular disease. Prev Chronic Dis. (2022) 19:E84. doi: 10.5888/pcd19.220347
PubMed Abstract | Crossref Full Text | Google Scholar
79. Birger, M, Kaldjian, AS, Roth, GA, Moran, AE, Dieleman, JL, and Bellows, BK. Spending on cardiovascular disease and cardiovascular risk factors in the United States: 1996 to 2016. Circulation. (2021) 144:271–82. doi: 10.1161/CIRCULATIONAHA.120.053216
PubMed Abstract | Crossref Full Text | Google Scholar

